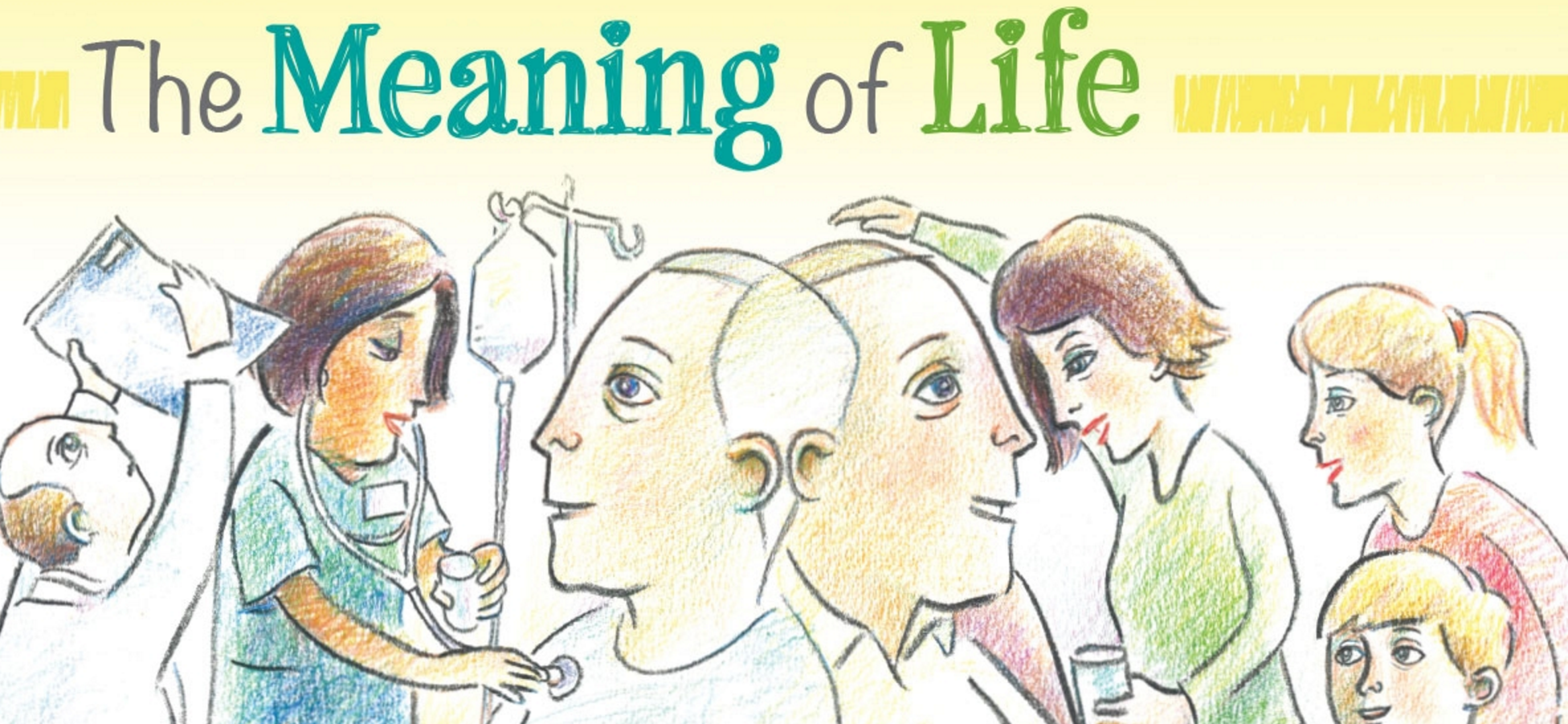
“I don’t know how to tell my family about the diagnosis…” “I haven’t told my kids that I’m dying…”
Families often reeling following the diagnosis of Cancer or other life-limiting diseases, struggle with how, and when, to have those essential conversations. I am a Social Worker and for the past 17 years have had the privilege of caring for people facing a life-limiting illness. It is an intimate and profound experience - sitting alongside people as they face end-of-life. They share their hopes and fears - about living and dying - and about caring for and leaving behind those they love. Trying to protect their families but also wanting to prepare them. Whether they speak lovingly about a partner, or children, or siblings, parents or best friends… grieving these losses begins at time of diagnosis.
While treating and managing the disease is important - equally important is caring for the person diagnosed with the disease. What is truly important to them? Who is important to them? How do we provide support in a manner that is congruent with their values and wishes? How do we normalize grief following a diagnosis, and in turn, sit alongside them creating safe spaces - and time - to share their grief should they so choose? As clinicians, we can facilitate supportive interventions at any stage of illness and ideally engage the entire family. Sadly, many families - and specifically many children and youth remain uninformed following the diagnosis of a life-limiting illness, largely resulting from parents need to “protect” and their fear of not knowing what to say. This phenomenon is not rare as it also extends to healthcare professionals, with many reporting fear and uncertainty as to how to best support grieving families and children. This is true whether a child has been diagnosed with a life-limiting illness, or the parent of a child has been diagnosed. Understandably, if the psychosocial needs of families, specifically children and youth remains unaddressed, it only serves to create additional distress for parents and caregivers.
As a Palliative Social Worker I recognize the importance of creating safe spaces and time to have these conversations - to support families in telling their stories, celebrating their connections, and should they so choose, to openly and collectively share their grief. A specific legacy project created opportunities for families to do just that - to hold on, while letting go. I have completed this project with many families facing a life-limiting disease - following diagnosis, throughout the illness, at end-of-life and following the death of a loved one. This can be completed with children of all ages and regardless of the make up of the family - large or small, we meet together and explore their understanding of the diagnosis, the impact of the illness while also celebrating and honouring connections. That Project? While the results have been profound, the activity is, quite simply, creating a “Hug”.
To be clear, this is not a professional boundary violation, but in fact, a creative legacy project that can be done by anyone, anywhere, at any time. In obtaining consent from parents and caregivers, I explain that this is an opportunity for the family to collectively talk about the illness, share stories and experiences, communicate concerns, dispel fears, foster support and enact plans. I introduce this activity as a symbol of their unending love – and the Hug can be taken anywhere - to chemo daycare, during an admission to hospital or hospice, or even once someone has died – this “hug” is also something that can be buried or cremated and remain with a loved one forever…
I assure you this experience is more than a creative activity - it is an intimate and collaborative experience for the family to create a lasting memory. While each experience is unique and the degree to which some “patients” may be able participate varies, in each situation, the family gently accommodates their loved one. What remains universal are the shared laughs, tears and a multitude of stories - reminders of shared experiences and memories of their lives together.
But perhaps I should explain… I feel it is important to outline the essential elements required for this intervention… Specifically, informed consent from the family, clean bed sheets, colourful markers, scissors and glitter. It is simply a matter of laying a sheet on the ground, then a family member lays down on the sheet while another family member traces their outstretched arms and outstretched fingers. After sitting up, lines are drawn to connect the tracings of each arm and then cut along the lines. Although tantamount to making a scarf – it is, more importantly the outstretched arms of their loved one, it is a personalized “Hug”. The child, or partner, sibling, parent or friend then adorns their hug with messages and images and reminders of the shared connection with their loved one - in essence, the “Hug” becomes a tangible expression of their love.
While I involved partners, children, siblings, cousins and friends in this activity long ago I wondered, what if their loved one (or the “patient”, to be clear) also wanted to reciprocate? I began asking patients about this and the suggestion of leaving this touching legacy was always met with resounding approval. While this always requires patient consent and discussion throughout, I have completed this activity with people who were ambulatory as well as people who were bed-bound. While collectively engaging the individual and family, for those who are bed-bound, we carefully slide a folded sheet behind the back of their loved-one. Throughout the activity, the family shares stories and memories, while tenderly helping to hold and trace the outstretched arms and fingers on each hand - every action and movement becomes an incredibly intimate experience. In the case of pathological fracture, we have used the singular tracing of one arm to make a mirror image - completing the hug. Taking that singular hug and laying sheets over top, additional copies are then traced for each family member. This not only engages entire families at the bedside, but also creates a lasting legacy for the surviving family. We often discuss sewing material from favourite blankets, shirts or sweaters on the reverse to preserve a tangible and personal connection.
I have completed this activity when families speak a language different from my own. Despite only being able to communicate through an Interpreter, the conversation remains seamless throughout as we create a beautiful and moving tribute for their family while they collectively support each other in their shared love and grief. While many young couples anticipate milestones like a wedding or the birth of a child, I have also facilitated this project at the bedside of the dying parent together with their young adult children, creating a space to share their hopes and stories while honouring their legacy. This supportive intervention has also bridged great distances, when families were thousands of miles apart. After completing the activity with the patient and family at the bedside, I encourage them to share the idea with extended family and friends across the country and in one specific case, family members of all ages from across the country made Hugs and sent them by courier to the bedside of their dying loved one. Their many colourful “Hugs” surrounded her when she died, each and every one told a story and was on display around her room as a meaningful and tangible connection. Much to the comfort of the family, each and every “Hug” was later buried with her. I have also completed this project with children following the death of a parent, it is especially important for those who were not informed about the illness or were unaware that death was expected. It is so essential to create a space for children to grieve alongside their families to share their thoughts, shed tears, and express the range of their feelings, including grief. We talk about what it feels like to receive hug from someone you love and the opportunity to create a lasting memento to leave with their parent as an expression of their unending connection. Although a parent - or any loved one might die before families and friends have an opportunity to say goodbye, we can still create opportunities for families to collectively share their love and express their sorrow while honouring the legacy of their loved one.
I believe as Health Care Professionals, we have an obligation to provide empathic person and family-centred care. From time of diagnosis we have an opportunity to facilitate honest communication, and in turn, promote adaptive coping strategies for those facing a life-limiting illness. In doing so, we can provide invaluable opportunities for families to connect, and collectively process experiences from time of diagnosis through to end-of-life, and into bereavement. I feel extraordinarily privileged that families allow me into their lives - to share their stories, their love and their grief. However brief our time may be together, I hold that time as sacred and do all I can to create a safe-space to foster these connections while honouring the legacy of those living and dying.