"The medicalization of death had arrived, one which for better or worse continues to shape how we die today."
Patients feel psycho-social impact of chemo more acutely than physical side effects
Highlighting the need for integrated Person and Family-Centred Care...
"The results show that there might be a gap between what doctors think is important or disturbing for patients, and what patients really think. Physical, psychological, social and spiritual support is needed at every stage of the disease"
Source: Patients feel psycho-social impact of chemo more acutely than physical side effects. MedicalXpress
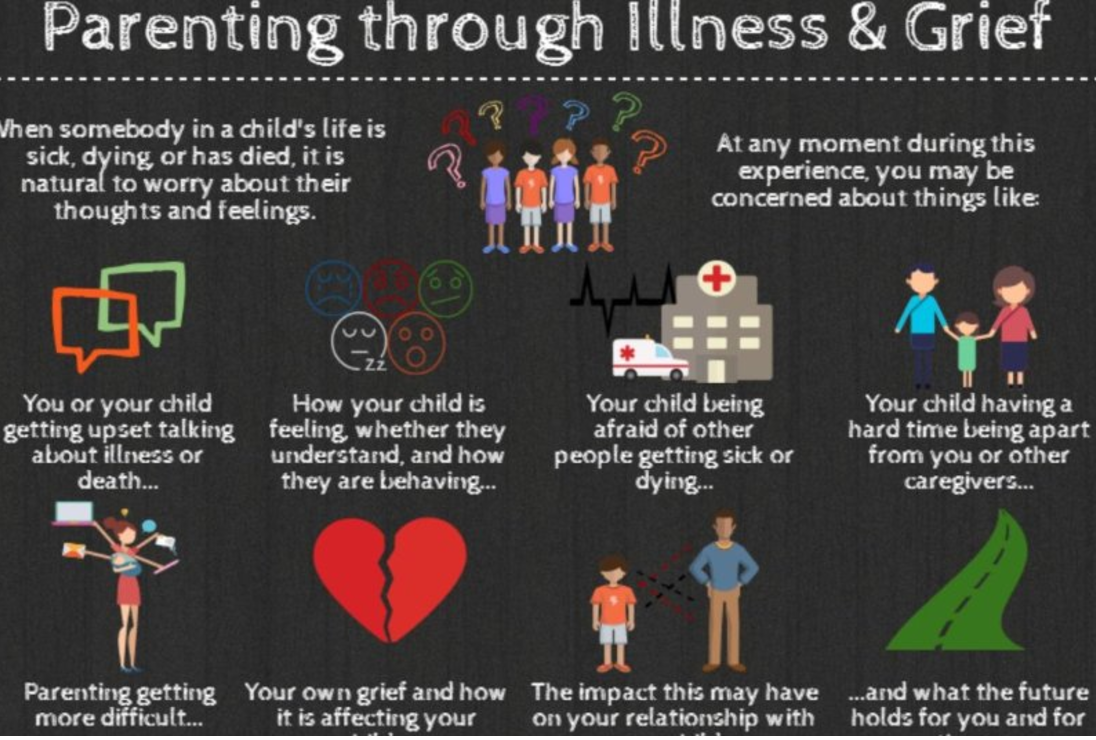
Parenting Through Illness & Grief
"This one page handout provides an overview of the findings from a research study of parent caregivers. The study was conducted as a collaboration between Dr. Jay Children`s Grief Centre and the Nanny Angel Network"
Source: Parenting Through Illness & Grief. Canadian Virtual Hospice
Grief In The Classroom: 'Saying Nothing Says A Lot'
" 'Virtually all children will go through it — but that doesn't mean it's a normalizing experience,' says Dr. David Schonfeld, an expert on student grief and a driving force behind the new website. 'Even though it's common, it warrants our attention.' "
The Coalition to Support Grieving Students
The Coalition to Support Grieving Students. A brilliant and essential collaboration to support #grieving #children #youth #teens
"...a groundbreaking, practitioner-oriented website designed to provide educators with the information, insights, and practical advice they need to better understand and meet the needs of the millions of grieving kids..."
When Death Moves In: grief after a death in the home
"In the years since we have worked with countless clients and families whose loved ones died at home. Some were anticipated hospice deaths. Others were unexpected, some traumatic. No matter the type of loss, time and again we hear people share their feelings that the deaths that occur in the home resides in the space. Even with the best and most dignified and supported of deaths, these memories and feelings in the space can sometimes feel overwhelming to manage.
We wish you could provide you the magic answer. We wish we had checklist of solutions that would clear your space of the difficult death memories to open the space for all the other, wonderful memories. Sadly, that isn’t how it works. What we can do is talk about some suggestions, tips, and ideas and think through the benefits and considerations..."
Source: When Death Moves In: grief after a death in the home. What's your Grief
Practising compassion in an uncompassionate health system. Hearts in Healthcare
"Yet, amidst the storm, some remarkable health professionals create a circle of calm. They go about their work in an unhurried way, finding time to greet their patients, put them at ease, listening deeply and offering kindness and compassion. They don’t neglect their clinical tasks, indeed they seem to get the work done with quiet efficiency. These inspiring workers go home with satisfaction and joy in their hearts. How is that possible?"
Source: Hearts in Healthcare Practising compassion in an uncompassionate health system
Death: A Part of Life. A 5-Part Mini Series (podcast)
Am honoured to have been a guest panelist on the final instalment of Death: A Part of Life - Part 5: The Grieving Process.
This informative 5-Part radio series with the Dr. Bob Kemp Hospice aired on CHML 900. Each week panelists including caregivers and healthcare professionals convened to open up a conversation about dying, death, grief and loss. The series explores issues such as: coping with the diagnosis of a serious illness; demystifying hospice palliative care; exploring available supports and services; advance care planning; the dying process and grieving which ultimately impacts us all.
The links to the podcasts of Death: A Part of Life are listed below:
Death, A Part Of Life - Part 1: Palliative Care.
It’s a fact of life that at one point we all will die. But is it all as simple as that? Bill Kelly and the Bob Kemp hospice will be discussing grief, relief and the acceptance of passing away. On today’s show we discuss what happens when you’re told you don’t have much time left, and whether healthcare is asking too much of caregivers, and whether people are prepared for palliative care.
Death, A Part Of Life - Part 2: Changes To Palliative Care.
For our second show, we will discuss what the palliative care system is now, how it works and what changes need to be made. What does one of our local MPPs hear from his constituents about healthcare and in particular, palliative care? How would changes affect patients? Does fear have a hold on how we make our decisions once we’re diagnosed as palliative? An example of this is whether to choose palliative care or medically assisted death.
Death, A Part Of Life - Part 3: Religion and Palliative Care.
We continue our series this week with two topics. The first one will be discussing the experience of death. Everyone treats death in our world differently. But is it strictly a medical experience or is it a spiritual one? In our second half, we will talk about access to palliative care services in various sectors of our society. How do we help the vulnerable and the community obtain access to proper palliative care?
Death: A Part of Life - Part 4: Bucket lists and preparation.
Life should be celebrated at all stages, whether it be infancy, adulthood and as life comes to a close. So how can we make the most out of life? How can those who are in palliative care achieve their “bucket list” dreams before they pass, and how does it apply when it comes to their own personal circumstances? How do we define a “bucket list”? How wise is it to be prepared for eventual health issues? How should we plan for advanced care and how does it affect the family? How do we navigate through the difficult decisions and pain to provide care for loved ones who are palliative?
Death: A Part of Life - Part 5: The grieving process.
The final instalment in our series sees us discussing grief and how this isn’t just an event that happens in life but a process that families have to go through. How do families grieve the loss of a loved one? How can we support one another and how does grief affect children?
Source: Global News. AM 900 CHML
Camp Erin: Where Children and Teens Learn to Grieve and Heal
Am honoured to volunteer with Camp Erin. It is indeed a remarkable community and one that nurtures capacity in children and youth to grieve the death of a loved one.
"Children and teens ages 6-17 attend a transformational weekend camp that combines traditional, fun camp activities with grief education and emotional support, free of charge for all families. Led by grief professionals and trained volunteers, Camp Erin provides a unique opportunity for youth to increase levels of hope, enhance self-esteem, and especially to learn that they are not alone.
Camp Erin is offered in every Major League Baseball city as well as additional locations across the U.S. and Canada. The Moyer Foundation partners with hospices and bereavement organizations to bring hope and healing to thousands of grieving children and teens each year.
Camp Erin allows youth to:
- Tell their story in a safe environment
- Process grief in healthy ways
- Meet friends facing similar circumstances
- Learn they are not alone
- Build a tool-box of coping skills
- Honor and memorialize loved ones
- Have fun!"
Source: Camp Erin. The Moyer Foundation
For information on Camp Erin locations in Ontario, please visit: Camp Erin Hamilton; Camp Erin Toronto; Camp Erin Eastern Ontario; Camp Erin Montreal
September 10th is World Suicide Prevention Day #WSPD
"Being caring and listening with a non-judgemental ear are far more likely to reduce distress than exacerbate it." https://iasp.info/wspd2017/
For support and resources please see:
World Suicide Prevention Day at https://iasp.info/wspd2017/
Canadian Mental Health Association at http://www.camh.ca/en/hospital/health_information/a_z_mental_health_and_addiction_information/suicide/Pages/default.aspx
What can Palliative Care Do?
"When you are facing a serious illness, you need relief from symptoms. You need to better understand your condition and choices for care. You need to improve your ability to tolerate medical treatments. And, you and your family need to be able to carry on with everyday life. This is what palliative care can do." #SeriousIllness #PalliativeCare
For more information visit Get Palliative Care
Camp Erin offers a weekend for kids coping with grief and loss
"We strongly believe that the Camp Erin experience is life-changing. Family members and caregivers experiencing their own grief, while simultaneously helping their child to grieve, are often overwhelmed and feel helpless. Grief left unchecked can lead to depression, behavioural issues, suicide and substance abuse.
Much of what is addressed at camp is the isolation kids feel around their grief; it is a poignant experience for the campers to have the chance to go away for three days, (oftentimes, these kids have never been up north) with other people their own age, forming a bond over their loss. Camp Erin is a safe place for young people to identify with other kids who are feeling the same emotions, including anger, worry, guilt and often, a "Why me?" outlook.
When kids come back from camp, at ease and with the confidence to talk about their grief, it gets passed along to their parents."
Full article: Camp Erin offers a weekend for kids coping with loss
Across the Continuum: The Need for Innovative Approaches to Person and Family-Centred Care
Was honoured to present Across the Continuum: The Need for Innovative Approaches to Person and Family-Centred Care, a H.I.T (Healthcare, Innovation, Technology) Talk at the Hospice Palliative Care Ontario 2017 Annual Conference "Accessing Compassionate Hospice Palliative Care Across the Continuum" (excerpt below).
From time of diagnosis so much is asked of those facing a life-limiting illness… Ultimately, they’re expected to “hold on” while also having to “let go”. How then can we consider innovative approaches to person and family-centred care across the continuum, at a time when healthcare providers are required to do more, with less?
I am honoured to say that I am a Social Worker, and there’s a phrase that rings true for me in the work that I do as I often step outside of my comfort zone. The idea of “leaning into the discomfort”. I’d like to reflect on why it’s important for every healthcare provider to consider the way we approach our work.
Working within a frenetic yet extraordinary healthcare system, we face time-constraints, the demand for evidence-based competencies, the expectation of metrics and outcome measures, people often referred to by a medical record number or identified by a disease… quite often, healthcare feels rushed and impersonal… As a result, healthcare providers may not fully engage because of increasing practice demands and time constraints, they may avoid certain experiences where they don’t feel competent or hesitate to go those places when faced with uncertainty…
In fact, much like life itself… acknowledging and meeting the challenges in the midst of uncertainty and chaos are really an integral part of our work. How then can we engage and enter those spaces when we feel that we don’t have time, when we don’t know the answers, or when we’re unsure of what we may find?
While the idea of creating and implementing innovations in practice may sound weighty, the definition of innovation is actually quite simple. Innovation is the introduction of something new… a new idea, method or device. That’s it. You don’t necessarily need to write a grant, or consider retraining, or apply to the research ethics board (and while that may be part of your innovation), introducing something new doesn’t have to be onerous, it can actually be something quite simple.
Hospice Palliative Care has always been ahead of the curve… in recognizing and valuing person and family-centred care, in acknowledging "total pain", in taking holistic approaches to supporting quality of life, to recognizing and integrating interprofessional collaboration. Innovations in Hospice Palliative Care remain essential today, and perhaps more so now than ever before.
At present, we’re faced with tremendous opportunity. With the quality of living and dying on our social and political landscape, with Bill C-277 (An Act providing for the development of a framework on Palliative Care in Canada) passed by the House of Commons, with the provincial and federal governments acknowledging the need for increased funding in Hospice Palliative Care… we’re on the precipice of change. How then can we be agents of change, and consider innovative approaches to person and family-centred care across the continuum - from time of diagnosis, throughout the trajectory of an illness, at end of life and into bereavement?
We face the reality that many people, including many healthcare providers, assume that Hospice Palliative Care is nothing more than a euphemism for end-of-life care. That presents us with an opportunity… to continue to advocate and educate about the remarkable scope and breadth of Hospice Palliative Care across the continuum. But in doing so, it’s also important to consider, when does dying begin, and how can we support people to live well during that process?
Does dying begin the moment we’re born? Or when a fatal condition begins? Is it when that condition is recognized by a physician, or it when nothing more can be done to reverse the condition or to preserve life? As we know, the answer to that question varies from one person to the next…
While many focus on the quality of dying, or on death as a singular event, isn’t the whole end-of-life experience informed by the people and the events leading up to that death?
It’s these processes that take place in the days, weeks, months and even years before the death that are of paramount importance and contribute to overall quality of life - and that’s where we, as a community of care providers, can have the greatest impact.
Healthcare providers are often inhibited by their anxieties about saying or doing the wrong thing. This is true for any clinician, beyond our formal training and education, we continually face new scenarios, challenging experiences and uncertainty… We need to step outside of our comfort zone, and with humility… explore person and family-centred innovative approaches to care in an effort to promote healing.
It’s a profoundly intimate experience when we are allowed to share that space with someone facing dying, death, grief and loss… that compassionate connection can transcend so many barriers, and sometimes, however momentarily, sometimes… it can even transcend suffering. That connection can be extraordinary.
I believe as Health Care providers in Hospice Palliative Care, we can continue to lean into our discomfort and remain open to uncertainty and to wonder. I believe, through our humility and vulnerability, we can create compassionate and innovative approaches to person and family-centred care, and in doing so, provide invaluable opportunities for people to connect, and collectively process experiences across the continuum - from time of diagnosis, through to end-of-life and into bereavement.
As Dr. Rachel Remen explains, "the most important questions don't seem to have ready answers. But the questions themselves have a healing power when they are shared. An answer is an invitation to stop thinking about something, to stop wondering. Life has no such stopping places; life is a process whose every event is connected to the moment that just went by. An unanswered question is a fine traveling companion. It sharpens your eye for the road".
We’ll always face challenges and uncertainty in our work, but we need to be invested in innovative approaches to person and family-centred care, because as Dr. B.J. Miller says "Quality of Life isn't a Consolation Prize".
What Flying Can Teach Us About Rising Above the Turbulence
“I wonder if we can find in our own heart our own pilot who will search for more calm airs. Could we move up or down a bit to find a more peaceful state of the heart? Do we buckle up and patiently persevere through the storms of life? Is the turbulence something to avoid and get over, or is it life itself? Part of life?
I know there is wisdom in looking at serenity, not at merely “transcending” the storm, but also in navigating life. We are never promised pure bliss, or perfectly smooth sailing. A mature spiritual life consists of being able to navigate the storms. This I know.
I do remember the teachings of Buddhism, reminding us that the muck that the lotus rises through sustains the flower. This I know.
But I also know that not all of these stages are equally good, equally nourishing, equally beautiful for our hearts. That there are in us, inside us, more peaceful skies. Somewhere higher, or deeper, in us there is also a calm and tranquil realm of the spirit. It is breathing with the serenity above the turbulent clouds that there are blue skies and the warm sun. It is the state of being one with the One, breathing with the Source of all the universe. And what majestic intimacy there is Here. Now.
That serene realm, above the clouds, is not There. It is here, right here already with us…”
Full Article: On Being
Hospice Palliative Care is about Living Well. Right to the End.
It's National Hospice Palliative Care Week and it is so important to demystify and destigmatize the incredible breadth and scope of Hospice Palliative Care.
Hospice Palliative Care is about Living Well. Right to the End.
Hospice Palliative Care is aimed at relieving suffering and improving the quality of life for persons who are living with, or dying from, advanced illness or are bereaved.
The goal of Palliative Care is to provide comfort and dignity for the person living with the illness, as well as the best quality of life for both this person and his or her family*.
Palliative Care services are helpful not only when a person is approaching death but also during the earlier stages of an illness. Palliative care may be combined with other treatments aimed at reducing or curing the illness.
*”family" is whoever the person says his or her family is.
For more information and resources regarding Hospice Palliative Care, please visit the Canadian Hospice Palliative Care Association.
The Wisdom of Uncertainty
“ ‘What we’re looking for is where we are.’
Can we learn to live in joy amongst all that this great unknowing has to offer? Jack guides us through some of the key principles of the awakened heart, encouraging an attitude of graciousness toward the mysterious nature of our existence.”
Full article at JackKornfield.com
What is Advance Care Planning?
Source: Speak Up Ontario
Informed Patient? Don’t Bet On It
"We’ve seen too many patients regret decisions that they made without fully understanding their options, or the possible outcome. We encourage our patients, and our colleagues, to be partners in what are often life-changing decisions about health care."
Read the full article The New York Times
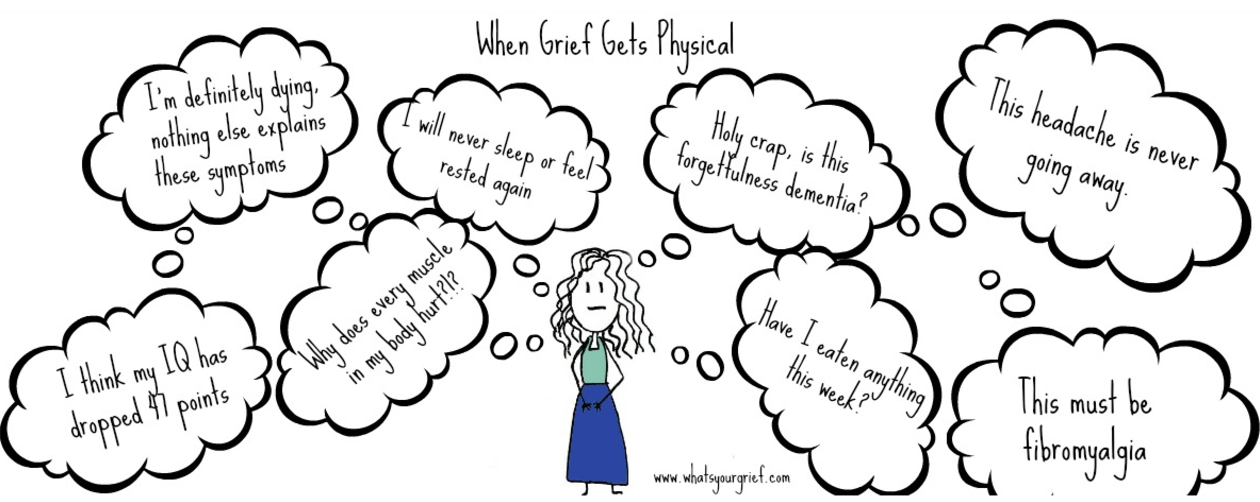
When Grief Gets Physical: dealing with physical grief symptoms
"There is simply no way to anticipate what grief feels like. It is one of those experiences that you can describe to someone, but it is impossible to really understand it until you are forced to live with it. Of all the unimaginable aspects of grief, there is one thing we hear people say time and again that they really didn’t expect: physical grief symptoms. They might not have been fully able to appreciate the emotional rollercoaster of grief until they were on it, but they at least had a sense it was part of the process. The physical stuff is something many people tell us they simply didn’t know to expect until it hit them like a ton of bricks.
When this happens, it can be distressing. Anytime we have new, uncomfortable physical issues it is distressing. But in grief that can sometimes be coupled with a new level of anxiety. In the past, a headache was a headache. After the devastating loss of a loved one, you are all-to-familiar with the reality that life can turn on a dime."
Read the full article at What's Your Grief
How to Die Well
"To start to find a way to experience a better end, we need to reflect on our own deaths and begin the process of accepting our mortality. This may happen through meditation, writing or conversations. Of course we should have hope if illness strikes us, but hope for perpetual life is blind. As we age or grow ill, the goal may switch from hope for longer life to hope for more attainable goals like healing relationships, living pain-free and enjoying a glass of Cabernet.
Simultaneously, we must prepare for this final stage of life. We must consider our preferences and values and shared them with our loved ones. Stephanie cared about being at home, with her family. What is most important to you? What would be most important to your loved ones? One day you might be called on to represent them. This conversation should happen repeatedly over the years, through the various stages of life and changes in health.
We must all — doctor, nurse, patient and family — also remember that these decisions require the collaboration of a whole team. The doctor is indeed the expert on the disease, but the patient is the expert on the patient. If you feel that you are not being included in decision-making for yourself or a loved one, or you don’t feel the team is communicating well, request a palliative care consultation, which brings communication expertise into the picture."
Read the full article at Time