" Families with unfinished business had significantly higher depression and grief scores after bereavement compared with those without."
Source: Unfinished Business in Families of Terminally Ill with Cancer Patients

" Families with unfinished business had significantly higher depression and grief scores after bereavement compared with those without."
Source: Unfinished Business in Families of Terminally Ill with Cancer Patients
"I tell them that it’s never my goal to glamorize death or tell people how they should or shouldn’t feel about death. I only hope my writing gives people permission to broach the topic."
Source: YES, I WRITE ABOUT DEATH: ON THE WAYS PEOPLE RESPOND TO A “DEATH JOB” AND HOW I HANDLE IT

"There is a cultural narrative that tells us that bad things don’t happen to good people. As a result, we spend a lot of time protecting kids from natural life events, like death."
Source: Joe Primo on Supporting Grieving Children. Option B

"Palliative care is the stance of being comfortable with the unknown, a stance that leads to the development of confidence, resilience, and empowerment in patients and families receiving the best care... we are all vulnerable, all subject to suffering, old age, and death..."

Highlighting the need for integrated Person and Family-Centred Care...
"The results show that there might be a gap between what doctors think is important or disturbing for patients, and what patients really think. Physical, psychological, social and spiritual support is needed at every stage of the disease"
Source: Patients feel psycho-social impact of chemo more acutely than physical side effects. MedicalXpress
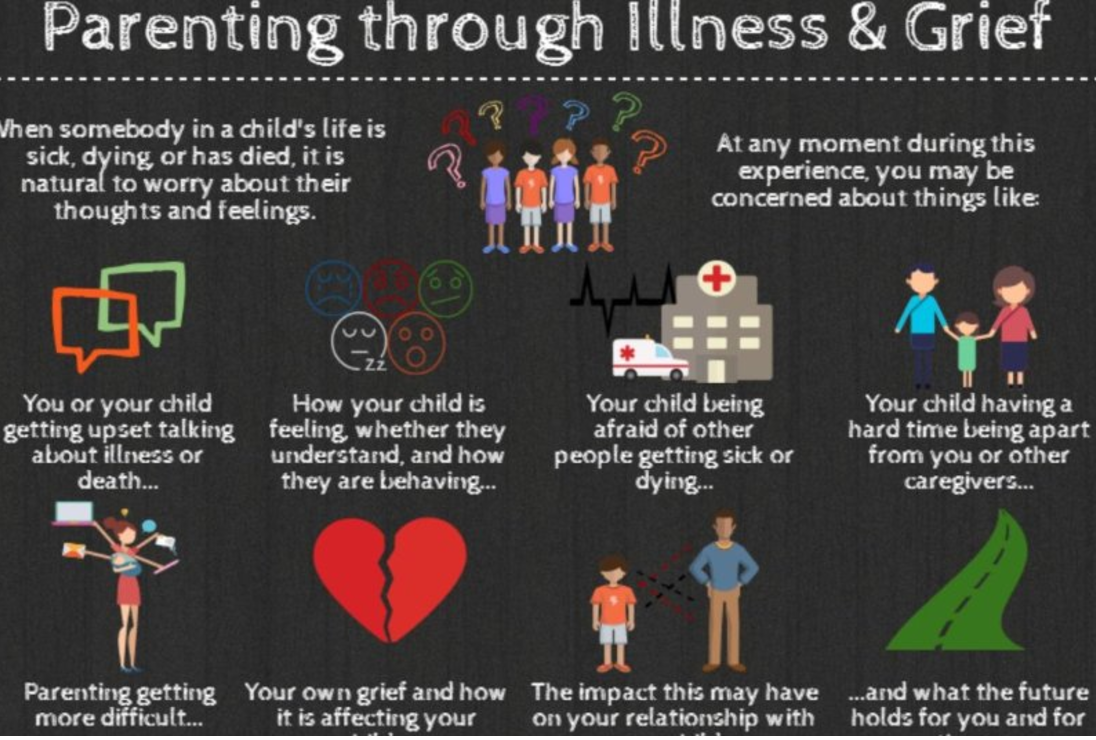
"This one page handout provides an overview of the findings from a research study of parent caregivers. The study was conducted as a collaboration between Dr. Jay Children`s Grief Centre and the Nanny Angel Network"
Source: Parenting Through Illness & Grief. Canadian Virtual Hospice

" 'Virtually all children will go through it — but that doesn't mean it's a normalizing experience,' says Dr. David Schonfeld, an expert on student grief and a driving force behind the new website. 'Even though it's common, it warrants our attention.' "
Am honoured to have been a guest panelist on the final instalment of Death: A Part of Life - Part 5: The Grieving Process.
This informative 5-Part radio series with the Dr. Bob Kemp Hospice aired on CHML 900. Each week panelists including caregivers and healthcare professionals convened to open up a conversation about dying, death, grief and loss. The series explores issues such as: coping with the diagnosis of a serious illness; demystifying hospice palliative care; exploring available supports and services; advance care planning; the dying process and grieving which ultimately impacts us all.

The links to the podcasts of Death: A Part of Life are listed below:
Death, A Part Of Life - Part 1: Palliative Care.
It’s a fact of life that at one point we all will die. But is it all as simple as that? Bill Kelly and the Bob Kemp hospice will be discussing grief, relief and the acceptance of passing away. On today’s show we discuss what happens when you’re told you don’t have much time left, and whether healthcare is asking too much of caregivers, and whether people are prepared for palliative care.
Death, A Part Of Life - Part 2: Changes To Palliative Care.
For our second show, we will discuss what the palliative care system is now, how it works and what changes need to be made. What does one of our local MPPs hear from his constituents about healthcare and in particular, palliative care? How would changes affect patients? Does fear have a hold on how we make our decisions once we’re diagnosed as palliative? An example of this is whether to choose palliative care or medically assisted death.
Death, A Part Of Life - Part 3: Religion and Palliative Care.
We continue our series this week with two topics. The first one will be discussing the experience of death. Everyone treats death in our world differently. But is it strictly a medical experience or is it a spiritual one? In our second half, we will talk about access to palliative care services in various sectors of our society. How do we help the vulnerable and the community obtain access to proper palliative care?
Death: A Part of Life - Part 4: Bucket lists and preparation.
Life should be celebrated at all stages, whether it be infancy, adulthood and as life comes to a close. So how can we make the most out of life? How can those who are in palliative care achieve their “bucket list” dreams before they pass, and how does it apply when it comes to their own personal circumstances? How do we define a “bucket list”? How wise is it to be prepared for eventual health issues? How should we plan for advanced care and how does it affect the family? How do we navigate through the difficult decisions and pain to provide care for loved ones who are palliative?
Death: A Part of Life - Part 5: The grieving process.
The final instalment in our series sees us discussing grief and how this isn’t just an event that happens in life but a process that families have to go through. How do families grieve the loss of a loved one? How can we support one another and how does grief affect children?
Source: Global News. AM 900 CHML

Am honoured to volunteer with Camp Erin. It is indeed a remarkable community and one that nurtures capacity in children and youth to grieve the death of a loved one.
"Children and teens ages 6-17 attend a transformational weekend camp that combines traditional, fun camp activities with grief education and emotional support, free of charge for all families. Led by grief professionals and trained volunteers, Camp Erin provides a unique opportunity for youth to increase levels of hope, enhance self-esteem, and especially to learn that they are not alone.
Camp Erin is offered in every Major League Baseball city as well as additional locations across the U.S. and Canada. The Moyer Foundation partners with hospices and bereavement organizations to bring hope and healing to thousands of grieving children and teens each year.
Camp Erin allows youth to:
Source: Camp Erin. The Moyer Foundation
For information on Camp Erin locations in Ontario, please visit: Camp Erin Hamilton; Camp Erin Toronto; Camp Erin Eastern Ontario; Camp Erin Montreal





“I wonder if we can find in our own heart our own pilot who will search for more calm airs. Could we move up or down a bit to find a more peaceful state of the heart? Do we buckle up and patiently persevere through the storms of life? Is the turbulence something to avoid and get over, or is it life itself? Part of life?
I know there is wisdom in looking at serenity, not at merely “transcending” the storm, but also in navigating life. We are never promised pure bliss, or perfectly smooth sailing. A mature spiritual life consists of being able to navigate the storms. This I know.
I do remember the teachings of Buddhism, reminding us that the muck that the lotus rises through sustains the flower. This I know.
But I also know that not all of these stages are equally good, equally nourishing, equally beautiful for our hearts. That there are in us, inside us, more peaceful skies. Somewhere higher, or deeper, in us there is also a calm and tranquil realm of the spirit. It is breathing with the serenity above the turbulent clouds that there are blue skies and the warm sun. It is the state of being one with the One, breathing with the Source of all the universe. And what majestic intimacy there is Here. Now.
That serene realm, above the clouds, is not There. It is here, right here already with us…”
Full Article: On Being

It's National Hospice Palliative Care Week and it is so important to demystify and destigmatize the incredible breadth and scope of Hospice Palliative Care.
Hospice Palliative Care is about Living Well. Right to the End.
Hospice Palliative Care is aimed at relieving suffering and improving the quality of life for persons who are living with, or dying from, advanced illness or are bereaved.
The goal of Palliative Care is to provide comfort and dignity for the person living with the illness, as well as the best quality of life for both this person and his or her family*.
Palliative Care services are helpful not only when a person is approaching death but also during the earlier stages of an illness. Palliative care may be combined with other treatments aimed at reducing or curing the illness.
*”family" is whoever the person says his or her family is.
For more information and resources regarding Hospice Palliative Care, please visit the Canadian Hospice Palliative Care Association.

“ ‘What we’re looking for is where we are.’
Can we learn to live in joy amongst all that this great unknowing has to offer? Jack guides us through some of the key principles of the awakened heart, encouraging an attitude of graciousness toward the mysterious nature of our existence.”
Full article at JackKornfield.com
Source: Speak Up Ontario

"We’ve seen too many patients regret decisions that they made without fully understanding their options, or the possible outcome. We encourage our patients, and our colleagues, to be partners in what are often life-changing decisions about health care."
Read the full article The New York Times
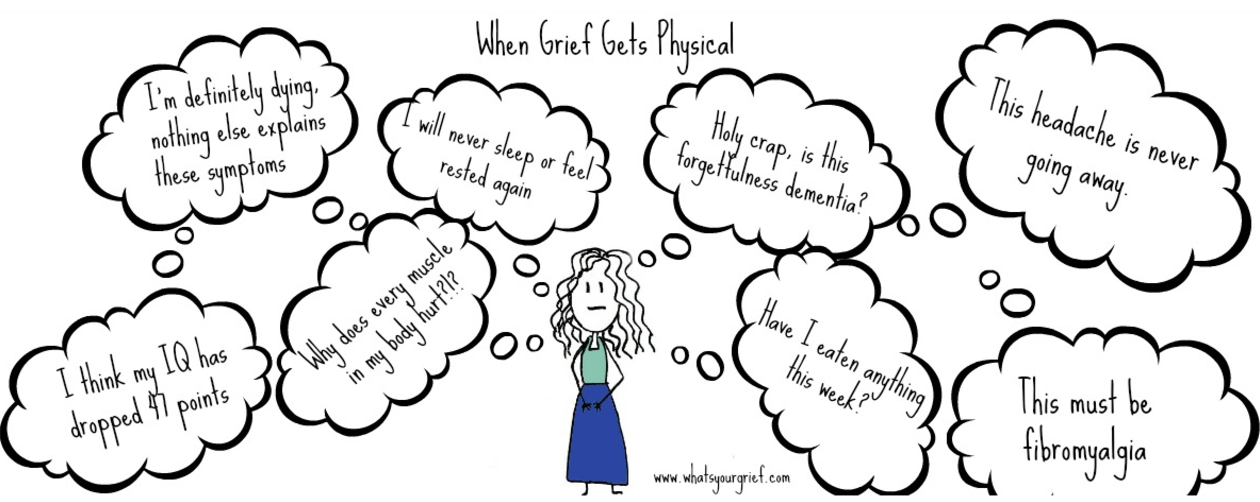
"There is simply no way to anticipate what grief feels like. It is one of those experiences that you can describe to someone, but it is impossible to really understand it until you are forced to live with it. Of all the unimaginable aspects of grief, there is one thing we hear people say time and again that they really didn’t expect: physical grief symptoms. They might not have been fully able to appreciate the emotional rollercoaster of grief until they were on it, but they at least had a sense it was part of the process. The physical stuff is something many people tell us they simply didn’t know to expect until it hit them like a ton of bricks.
When this happens, it can be distressing. Anytime we have new, uncomfortable physical issues it is distressing. But in grief that can sometimes be coupled with a new level of anxiety. In the past, a headache was a headache. After the devastating loss of a loved one, you are all-to-familiar with the reality that life can turn on a dime."
Read the full article at What's Your Grief

"To start to find a way to experience a better end, we need to reflect on our own deaths and begin the process of accepting our mortality. This may happen through meditation, writing or conversations. Of course we should have hope if illness strikes us, but hope for perpetual life is blind. As we age or grow ill, the goal may switch from hope for longer life to hope for more attainable goals like healing relationships, living pain-free and enjoying a glass of Cabernet.
Simultaneously, we must prepare for this final stage of life. We must consider our preferences and values and shared them with our loved ones. Stephanie cared about being at home, with her family. What is most important to you? What would be most important to your loved ones? One day you might be called on to represent them. This conversation should happen repeatedly over the years, through the various stages of life and changes in health.
We must all — doctor, nurse, patient and family — also remember that these decisions require the collaboration of a whole team. The doctor is indeed the expert on the disease, but the patient is the expert on the patient. If you feel that you are not being included in decision-making for yourself or a loved one, or you don’t feel the team is communicating well, request a palliative care consultation, which brings communication expertise into the picture."
Read the full article at Time

"...Today, I can say that, of course, my life was permanently changed by losing Eric, but I know it is possible to make a new life that is rich and satisfying — though often tinged with sadness.
Now I find myself going and doing and functioning, and taking joy in life and its challenges. I never believed that would be possible, but I assure you it is. There are still times, especially good times, when the pain of missing Eric stops me in my tracks. But there are good times.
I believe I have grown in my ability to be compassionate and to understand the pain that others may be experiencing. Once you know the pain of excruciating, incomprehensible loss, you can’t un-know it. But when you endure struggle, you can also learn empathy.
I am sharing this because until I was diagnosed and treated with complicated grief — which I had never even heard of before and which 7 percent of bereaved people struggle with — I felt isolated and like my life had no meaning. I hope my story will reach anyone who’s feeling like that and show them there is hope. I even appeared on CBS to spread the word about complicated grief and help others who may be struggling. The Center for Complicated Grief has a website and can be found here."

"What’s often overlooked is that the simple conversation between doctor and patient can be as potent an analgesic as many treatments we prescribe."

“ ‘Because by that time the patient is too sick to be able to have a voice in their own care, their family members have never had this discussion with the patient because no one guided them,’ said Periyakoil. ‘So as a result, they're sort of making these very high stakes decisions in the dark. They, because they love the patient so much, are caught up in the deep, emotional trauma and it's very hard for them to be able to make decisions.’
If family members can’t speak on behalf of the patient, Periyakoil says aggressive, heroic measures will generally be used to prolong the patient’s life.
‘The system default is to do everything possible, every treatment possible, even though the treatment might be ineffective and the treatment may be something the patient doesn't want,’ said Periyakoil.”

“People have concerns besides simply prolonging their lives. Surveys of patients with terminal illness find that their top priorities include, in addition to avoiding suffering, being with family, having the touch of others, being mentally aware, and not becoming a burden to others. Our system of technological medical care has utterly failed to meet these needs, and the cost of this failure is measured in far more than dollars. The hard question we face, then, is not how we can afford this system’s expense. It is how we can build a health-care system that will actually help dying patients achieve what’s most important to them at the end of their lives.”