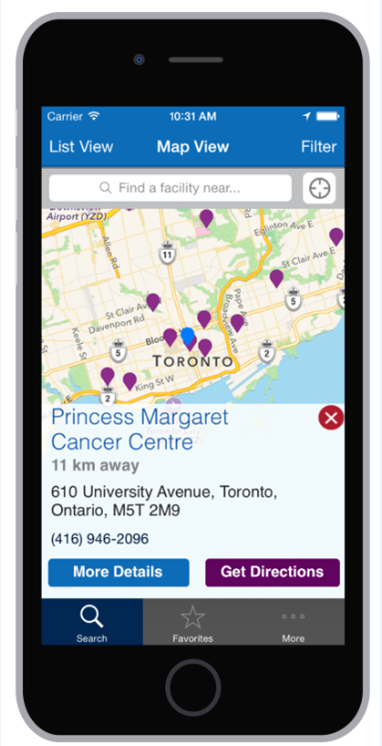
"Lead researcher Dr. Camilla Zimmermann, head of the palliative care program at Princess Margaret Hospital, says there is a misconception about what palliative care is.
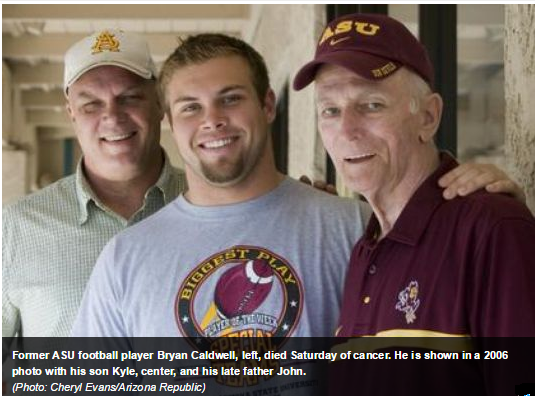
Many people believe it is the type of care hospitals offer when they have exhausted all medical options. They think it means that the oncology teams, having run out of cancer fighting tools, then hand off patients to people specialized in helping ease the final days of a dying person's life.
As a result, Zimmermann says, some people are reluctant to avail themselves of the help palliative care teams offer earlier in their cancer journey.
She says palliative care teams — some of which have started to call the service they offer supportive care — collaborate with oncology teams to try to help patients through difficult treatments and the progression of their illness. For the palliative care team, that can mean providing access to home care and to assessments of the needs of the patient and his or her family, among other things.
The aims of both teams are the same, Zimmermann says — prolonging life and improving quality of life".