"The essential guide for every patient and family.
When you are diagnosed with a life-changing illness, it can be overwhelming. While your diagnosis cannot be changed, the way you experience your illness can.
In Hope for the Best, Plan for the Rest, we draw on our decades spent researching and caring for thousands of seriously ill patients to reveal the seven keys for a better illness experience. With real-life stories, tips, and exercises to improve your journey right from diagnosis, we want to empower you with practical tools to navigate the healthcare system with knowledge, confidence, and clarity.
You can find hope in the face of uncertainty. You can live well, be fully informed, and be activated - and feel more like a person and less like a patient. But most of all, you can be hopeful and prepared at every step along the way."
Source: Waiting Room Revolution
Holding Exquisite Presence When Supporting Children and Their Families Who are Grieving
I was incredibly honoured to join my compassionate friend and dear colleague, Rami Shami, in a creative space, talking about the need for grief to come out of the shadows.
“How we support children and youth in their grief can have a lasting impact on their mental, emotional, even physical health. Joining us on this podcast is an individual who draws on her knowledge and experiences as an educator, a clinician in private practice, and a mother, in sharing how to hold what she calls, 'exquisite presence,' when supporting children and youth who are grieving. Her approach, garnered through decades of in the field work within numerous settings, highlights practical and informative insights into the disenfranchisement of grief amongst children, and how promoting safe spaces can help children process their experiences of loss. Join us for an exceptional informative and educational podcast!”
Source: The Lighthouse Beacon Podcast
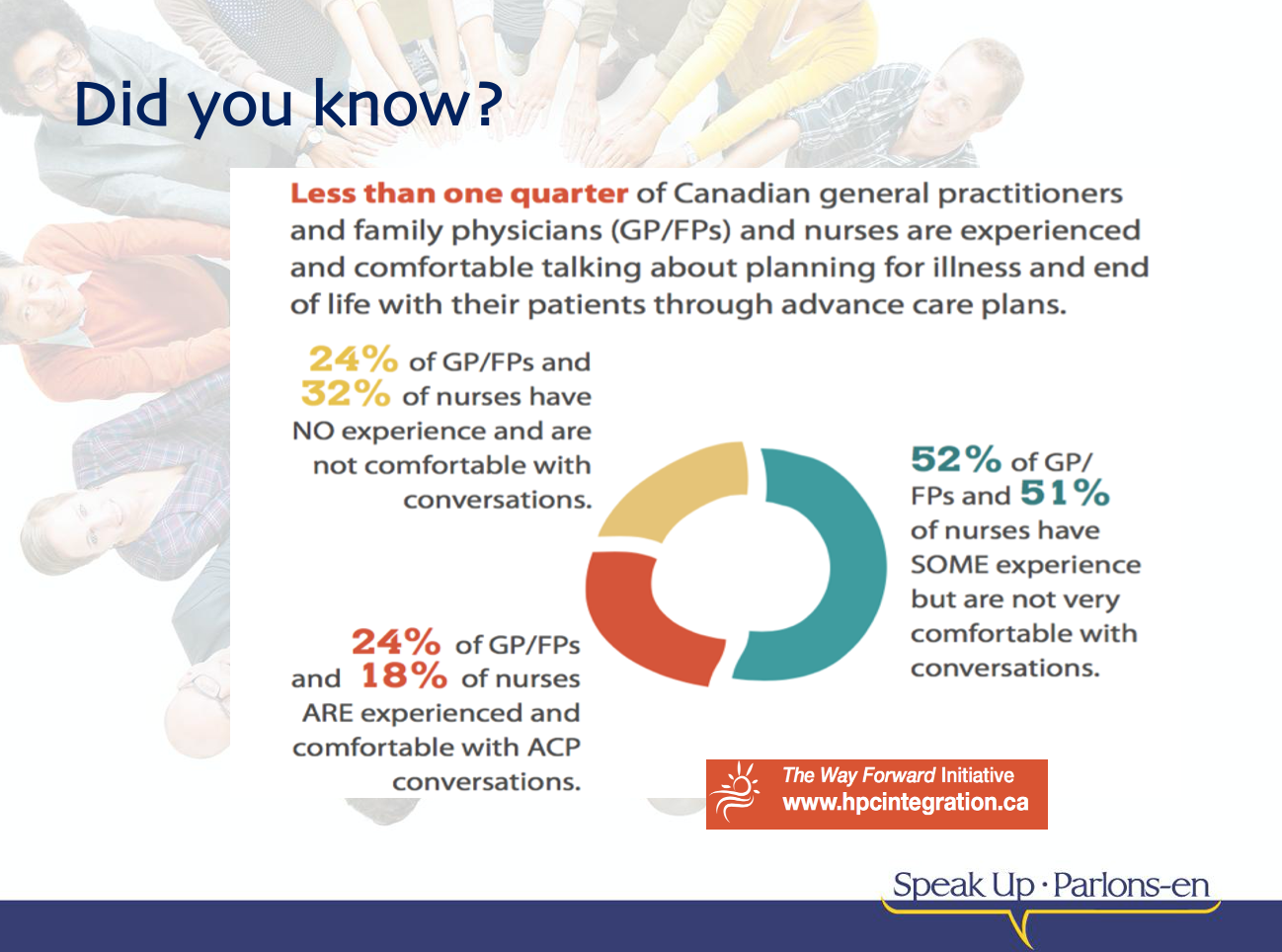
April 16th is Advance Care Planning Day in Canada
Planning for future healthcare needs is important.
Who would you trust to make healthcare decisions?
Do you know what would happen if you couldn’t communicate for yourself?
Who would you trust to make those healthcare decisions on your behalf?
Think about:
Who you would trust with making important decisions for you.
What matters most in your life and how that might help guide healthcare decisions you would want.
Consider:
Do you know what would happen if you couldn’t decide for yourself?
Who do you trust to make healthcare decisions that respect your wishes?
Would that person (or people) be able to make important decisions about your health in an emergency?
Have you spoken to anyone about what matters most in your life?
What gives you strength in difficult times?
Are spiritual, cultural or religious beliefs, practices, or ceremonies are important to you?
The best time to think about this is NOW (in advance of a medical crisis), while you can make decisions and communicate for yourself. You have the power to choose who that person is. They can be a family member, a friend, or anyone in your life that you trust to make the kinds of healthcare decisions you would want.
Ask yourself: If not you, who?
Source: Advance Care Planning Canada
It is never too early, but it can be too late!
To learn more about Advance Care Planning in 5 Steps, visit Advance Care Planning Canada to access helpful free toolkits and guides to help you along the way.
FREE Death Café at the David Braley Health Sciences Centre, McMaster University
In celebration of Advance Care Planning Day 2024, I am honoured to co-facilitate a FREE Death Café at the David Braley Health Sciences Centre, together with Dr. Alan Taniguchi, McMaster University on behalf of The 100% Certainty Project. Death: Something to Talk About.
Registration is required for this FREE Death Café on Wednesday March 27th (6-8pm) via Eventbrite
Death Café is an international movement where people, often strangers, gather to eat, drink tea and discuss death. The objective is 'to increase awareness of death with a view to helping people make the most of their (finite) lives’.
At Death Café, you can expect a group directed discussion of death with no agenda, objectives or themes. It is a discussion group. Please note that Death Café is NOT a grief support group, nor is this a grief counselling session.
Death Café is a respectful, public event where people of all communities and belief systems are welcome to have respectful discussions about death.
Interesting conversation is guaranteed! For more information, please visit Death Café
FREE Death Café at McMaster University: August 9th (6-8pm)
I am honoured to facilitate a FREE Death Café on Wednesday August 9th (6-8pm) at the David Braley Health Sciences Centre, McMaster University on behalf of The 100% Certainty Project. Death: Something to Talk About.
Registration is required for this FREE Death Café via Eventbrite at: https://www.eventbrite.ca/e/death-cafe-tickets-668976405437
Please note: Death Café is an international movement where people, often strangers, gather to eat, drink tea and discuss death. The objective is 'to increase awareness of death with a view to helping people make the most of their (finite) lives’.
At Death Café, you can expect a group directed discussion of death with no agenda, objectives or themes. It is a discussion group. Please note that Death Café is NOT a grief support group, nor is this a grief counselling session.
Death Café is a respectful, public event where people of all communities and belief systems are welcome to have discussions about death. Interesting conversation is guaranteed! For more information, please visit Death Café https://deathcafe.com/
FREE Advance Care Planning (ACP) workbooks
April 16th is National Advance Care Planning Day in Canada
“If Not You, Who? Who would you trust to make your healthcare decisions? Planning for your future healthcare needs is important. So, we’re asking: Do you know what would happen if you couldn’t speak for yourself? Who would you trust to make those #healthcare decisions for you?
You have the power to choose who that person is. They can be a family member, a friend, or anyone in your life that you trust to make the kinds of healthcare decisions you would want.
Think about who you would trust with making those important decisions for you.
Think about what matters most in your life and how that might help guide someone in making the kinds of healthcare decisions you would want.
The best time to think about this is now when you can speak for yourself. We have useful guides to help you along the way.
Choosing a Substitute Decision-Maker (SDM)
Advance Care Planning policies can vary dependent on your province or territory. In order to ensure your end of life wishes are honoured it is crucial to have an understanding of your province or territory policies. This includes understanding what your #rights and #privileges are, as well as understanding the laws and regulations regarding end of life care, specific to your province or territory. While creating your advance care plan it is also important to make sure that you are using the correct documents for your province or territory.
Who do you trust most to make decisions for your health care that follow your wishes?
Would that person be comfortable with making important decisions about your health quickly or in an emergency?
Have you spoken to them about what matters most in your life? When someone knows what you value most in your life, they can make more informed decisions about your health care.
What Matters Most? What does a good day look like for you?
What situations do you find difficult?
What gives you strength in difficult times?
What spiritual, cultural or religious beliefs, practices, or ceremonies are important to you?
What do you value more: the possibility of a longer life, or the possibility of a better quality of life?
These questions can help guide you and your substitute decision-maker and assist them to prioritize what matters most to you when weighing care options.
April 16th is Advance Care Planning Day. So, ask yourself: If not you, who?”
Source: Advance Care Planning Canada
There are multiple FREE Advance Care Planning (ACP) workbooks, toolkits and guides specifically created to follow the provincial/territorial requirements for your advance care plan. Visit for FREE FREE Advance Care Planning (ACP) resources across Canada https://www.advancecareplanning.ca/acp-across-canada/
April 16th is National Advance Care Planning Day in Canada.
It’s about conversations. It’s about wishes. It’s how we care for each other.
Advance Care Planning is about having conversations with family and friends, especially your Substitute Decision Maker – the person who will speak for you if you cannot speak for yourself in case of a health emergency. It may also include writing down your wishes, and talking with healthcare providers and financial or legal professionals.
Advance care planning is a process of reflection and communication, a time for you to reflect on your values and wishes, and to let others know your future health and personal care preferences in the event that you are unable to consent or refuse treatment or other care.
Think about what is most important to you – your values, wishes and beliefs.
Learn about your overall health. This may include current conditions you want to better understand.
Decide on your Substitute Decision Maker(s), one or more people who are willing and able to speak, for you if you cannot speak for yourself.
Talk about your values, beliefs and wishes with your Substitute Decision Maker(s), family, friends and health care providers.
Record your values, wishes and beliefs in your Advance Care Planning Guide, in a letter, poem, video or audio recording.
Source: Advance Care Planning Canada
ADDITIONAL RESOURCES:
For more information on advanced illness, advance care planning, palliative care, end-of-life care and grief, please visit:
Canadian Virtual Hospice www.virtualhospice.ca
Living My Culture www.livingmyculture.ca
Advance Care Planning Canada values a free, accessible and open shared knowledge amongst the community. The website provides you with all the necessary tools to inform yourself on the most recent advanced care planning updates and developments. For more information and FREE resources, visit: https://www.advancecareplanning.ca/
April 16th is Advance Care Planning Day in Canada
April 16th is National Advance Care Planning Day in Canada, a day to promote conversations about your wishes and values for your future health and personal care in the event that you are unable to communicate for yourself. This year’s #ACPDay2021 is based on the theme "Advance Care Planning: An Essential Conversation for Everyone".
The ACP in Canada website - https://www.advancecareplanning.ca/acpday/ - features FREE downloadable resources, including posters and social media graphics for organizations and individuals across Canada to promote ACP.
Canadians have spoken, and although 80% of the population believes Advance Care Planning is important, less than 1 in 5 Canadians have an Advance Care Plan. Fortunately, the ACP website at www.advancecareplanning.ca is full of free information, tools, and conversation starters to help with starting the conversation. There are also links to provincial and territory-specific ACP resources across Canada.
How are you connecting with friends and family during these times? #ACPinCanada.
A Conversation... About Advance Care Planning, Life, Love, Loss & Legacy
SO grateful to have this conversation about Advance Care Planning, Life, Love, Loss & Legacy with Laurel Gillespie at Advance Care Planning Canada with the Canadian Hospice Palliative Care Association.
Creating safe spaces for people to have informed conversations about wishes and values is so important. Exploring and honouring connections and meaning for any individual and family in the face of illness and loss can be invaluable.
Please join us for a discussion about these invaluable conversations, while also exploring ways to connect with healthcare providers, and most certainly, with those we love.
Consider who, and what, gives your life meaning? Not just at the end of life, but now. It’s never too soon, but it can be too late.
Click here to listen to this episode of “A Conversation With…”
FREE Advance Care Planning Webinar
This FREE webinar will demystify Advance Care Planning in Canada and explore the stigma alongside some common barriers. We will dive into better understanding of Advance Care Planning and why it is relevant for EVERYONE, especially now. Lastly, free national resources will be provided to assist in beginning these essential conversations.
CLICK HERE to watch the full presentation.
Death Cafe for healthcare professionals, health science students or healthcare volunteers
Excited to be facilitating another Death Cafe for the Division of Palliative Care, McMaster Faculty of Health Sciences at McMaster University.
If you are a Healthcare Provider, Health Science Student, Hospice Palliative Care Volunteer or Funeral Service Employee, this Death Cafe is specifically for you!
A Death Cafe is a group directed discussion of death with no agenda, objectives or themes. It is a discussion group rather than a grief support or counselling session. The objective is 'to increase awareness of death with a view to helping people make the most of their (finite) lives'. Source: Death Cafe
Please join us at this FREE event at the David Braley Health Sciences Centre on Wednesday, July 24th from 6-8pm as part of our Public Health Palliative Care Elective.
Please help spread the word. While the event is free, registration is required via Eventbrite: https://www.eventbrite.ca/e/death-cafe-tickets-62361840945?fbclid=IwAR2aqlWTC8CcDPU4TKspXU3hZC65Om4ZxZZikvgh9ztqz3TEUe9GJcFLJ00
Talking About Death Won't Kill You: The 100% Certainty Project
"Most of us are ill-prepared to face what lies ahead. In a death-denying society, how do we ready ourselves for our human fate? How do we prepare for the end of our lives?
To this end, The 100% Certainty Project uses books to spark dialogue amongst citizens with the hope that grassroots efforts begin to build the social fabric we all will need at end-of-life. The project attempts to de-medicalize the experience of death & dying and engage community agencies and activists. We encourage the public to read and talk about books – books with themes of death, dying, bereavement, and loss. By facilitating conversation at dining room tables, in coffee shops and on street corners across Greater Hamilton and beyond, this reading initiative aims to increase public awareness about death & dying and lessen society’s discomfort facing death." Source: The 100% Certainty Project
Please join us for the first in a series of FREE public events. As part of the Division of Palliative Care at McMaster University with McMaster Faculty of Health Sciences, and our "The 100% Certainty Project. Death: Something to Talk About" initiative, together with Heart House Hospice, am honoured to co-host and moderate this event at the Mississauga Library with my brilliant friend and colleague Dr. Kathy Kortes-Miller. While the event is free, registration is required via the Mississauga Public Library at (905) 615 4835.
In support of National Hospice Palliative Care Week, we'll hear about her experiences as a parent and spouse facing a cancer diagnosis, as a Social Worker in Palliative Care and as an academic researcher and educator. At this event, Kathy will share her insight and explore some of the big questions about living and dying. We'll also open up the conversation to the audience - questions are welcome. Please email questions in advance to our "100% Certainty" email address: talkaboutdeath100@gmail.com or, join us and ask Dr. Kortes-Miller directly. Her book "Talking About Death Won't Kill You. The Essential Guide to End-of-Life Conversations" will also be on sale at each event.
Please join us for this FREE public event. As part of the Division of Palliative Care with McMaster Faculty of Health Sciences, and our "The 100% Certainty Project. Death: Something to Talk About", am honoured to co-host and moderate this event at the Hamilton Public Library with my brilliant friend and colleague Dr. Kathy Kortes-Miller. While the event is free, registration is required via Eventbrite
Please join us for this final evening in our series of FREE public events. As part of the Division of Palliative Care at McMaster Faculty of Health Sciences, and our "The 100% Certainty Project. Death: Something to Talk About", together with Carpenter Hospice, am honoured to co-host and moderate this event at the Burlington Public Library with my brilliant friend and colleague Dr. Kathy Kortes-Miller. While the event is free, registration is required via the Burlington Public Library at (905) 639 3611.
EXPLORING GRIEF AND LOSS LITERACY: SUPPORTING AND EMPOWERING SCHOOL COMMUNITIES
Am thrilled to be offering a full-day of training on Feb. 1st for the Halton District School Board on “EXPLORING GRIEF AND LOSS LITERACY: SUPPORTING AND EMPOWERING SCHOOL COMMUNITIES”
Will be honoured to be present with so many professionals as we spend the day exploring:
- Grief and Loss Literacy (related to dying, death and non-death losses)
- Stigma Related to Illness, Dying, Grief
- The Dialogue of Loss
- Support Across School Communities
- Promoting Capacity & Engagement
- Opportunities for Self-Care
Looking forward to sharing some brilliant resources!
Communication and Connection for Families Coping with Cancer
I am honoured to have been a guest on this week’s VoiceAmerica - Live Internet Talk Radio Breast Friends Cancer Support Radio Network. Becky Olson and Sharon Henifin of Breast Friends of Oregon, both breast cancer survivors and thrivers have asked me to be their guest to discuss "Communication and Connection for Families Coping with Cancer", demystifying Palliative Care and highlighting the need to support individuals and families of all ages, from time of diagnosis through to bereavement. At the conclusion of our episode, I highlighted the National Hospice and Palliative Care Organization and Canadian Hospice Palliative Care Association as sources of information for people wanting to learn more about Palliative Care in the U.S. and Canada.
Breast Friends is a nonprofit organization started by Sharon and Becky so that no woman would feel alone on her journey and to provide needed resources to those facing the challenge of breast cancer, as well as to their families and friends. Please visit their website for more information: www.BreastFriends.org.
This episode aired live and is now archived at https://www.voiceamerica.com/episode/106520/communication-and-connection-for-families-coping-with-cancer
Unfinished Business in Families of Terminally Ill with Cancer Patients
" Families with unfinished business had significantly higher depression and grief scores after bereavement compared with those without."
Source: Unfinished Business in Families of Terminally Ill with Cancer Patients
YES, I WRITE ABOUT DEATH: ON THE WAYS PEOPLE RESPOND TO A “DEATH JOB” AND HOW I HANDLE IT
"I tell them that it’s never my goal to glamorize death or tell people how they should or shouldn’t feel about death. I only hope my writing gives people permission to broach the topic."
Source: YES, I WRITE ABOUT DEATH: ON THE WAYS PEOPLE RESPOND TO A “DEATH JOB” AND HOW I HANDLE IT
10 Things My Chronic Illness Taught My Children
"All three of us work to maintain balance — knowing when we need to flex and when we need to release, when to put pain first and when to let it fade into the moment."
Patients feel psycho-social impact of chemo more acutely than physical side effects
Highlighting the need for integrated Person and Family-Centred Care...
"The results show that there might be a gap between what doctors think is important or disturbing for patients, and what patients really think. Physical, psychological, social and spiritual support is needed at every stage of the disease"
Source: Patients feel psycho-social impact of chemo more acutely than physical side effects. MedicalXpress
Grief In The Classroom: 'Saying Nothing Says A Lot'
" 'Virtually all children will go through it — but that doesn't mean it's a normalizing experience,' says Dr. David Schonfeld, an expert on student grief and a driving force behind the new website. 'Even though it's common, it warrants our attention.' "
Practising compassion in an uncompassionate health system. Hearts in Healthcare
"Yet, amidst the storm, some remarkable health professionals create a circle of calm. They go about their work in an unhurried way, finding time to greet their patients, put them at ease, listening deeply and offering kindness and compassion. They don’t neglect their clinical tasks, indeed they seem to get the work done with quiet efficiency. These inspiring workers go home with satisfaction and joy in their hearts. How is that possible?"
Source: Hearts in Healthcare Practising compassion in an uncompassionate health system