I was honoured to present "Navigating the Impact of Complex Illness as a Caregiver" during National Hospice Palliative Care Week to VON Canada Grey Bruce, Supportive Care Program and an incredible group of Caregivers and Care Providers.
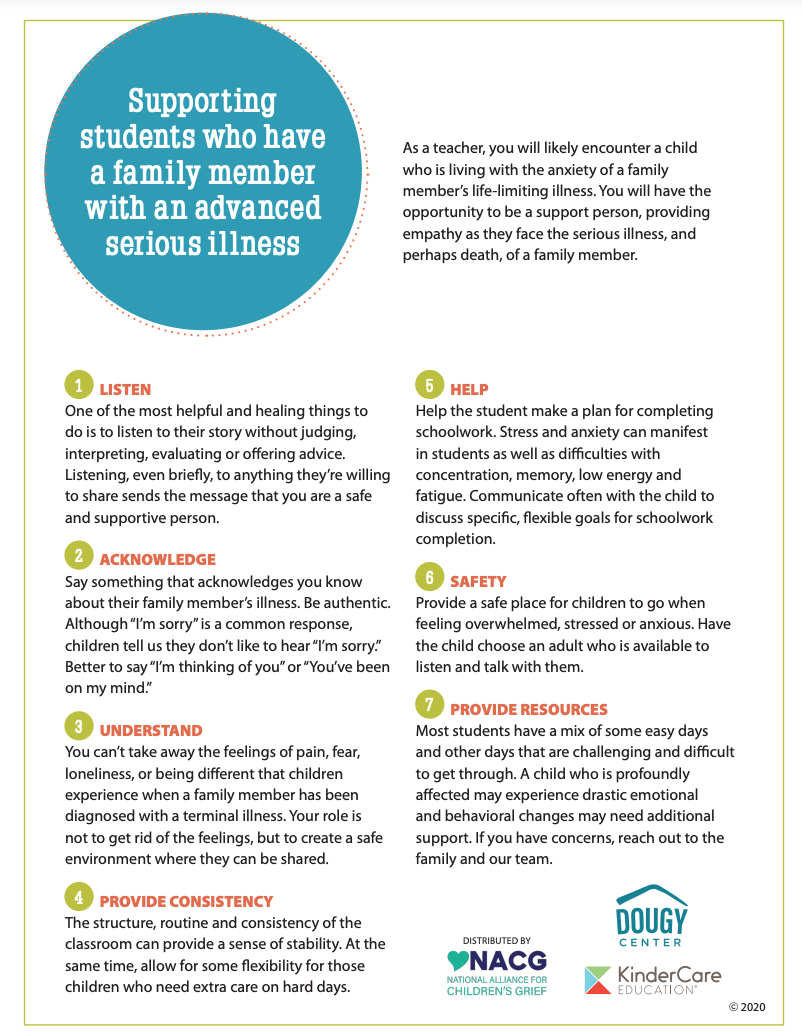
Following the diagnosis of a complex illness, it is common for family to feel a range of emotions including sadness, anxiety, anger and hopelessness. Facing these challenges can sometimes bring people together, while often, it can feel like it pulls people apart. Caregiving requires balancing multiple roles and stressors, while also navigating grief and uncertainty.
Caregiving can feel isolating and often means losses of identity, ritual and connections. Navigating the changes and uncertainty as a caregiver is part of the added demands of an illness experience.
Harris (2016) states, "Grief is a response to disorganization that occurs after an assumption about the world is challenged by a significant loss. Conflict occurs between assumptions & situations that challenge those assumptions. Grieving is the process of how the new assumptive world is (re)formed over time"
Yet, amid all the challenges and changes, grief is carried and often unaddressed. Most assume it happens only once someone is dying or has died. So much non-death loss and grief occurs throughout our lifetime, especially following the diagnosis of a complex illness, throughout the illness experience, at time of death, and for the balance of our lives as we (re)form the world around us.
Caring in Canada (May 2024) via Canadian Centre for Caregiving Excellence provides results from the National Caregiving Survey of 3,000 Caregivers and Care Providers highlighting:
- Caregiving takes a toll on a caregiver’s wellbeing
- Caregivers are working ‘extra-shifts’
- Caregivers 65+ also need care
- Caregiving has a financial toll
- Care provider shortage is linked to poor working conditions
- Diverse communities face barriers and gaps in support
Integrated and accessible support is needed for caregivers throughout the illness experience.
*Family is best defined by the person receiving care. It can include family of origin, or chosen family.