CGAD seeks to raise awareness of the painful impact that the death of a loved one has in the life of a child or teen, and provides an opportunity to make sure that these children and #teens receive the support they need. In just one year, over 203,000 of Canada’s 7.5 million youth under 18 will experience the death of someone in their extended family.
1 out of every 14 children and teens will experience the death of a #parent, #caregiver or #sibling who lives in their home. These youth experience the ripple effect of multiple losses…
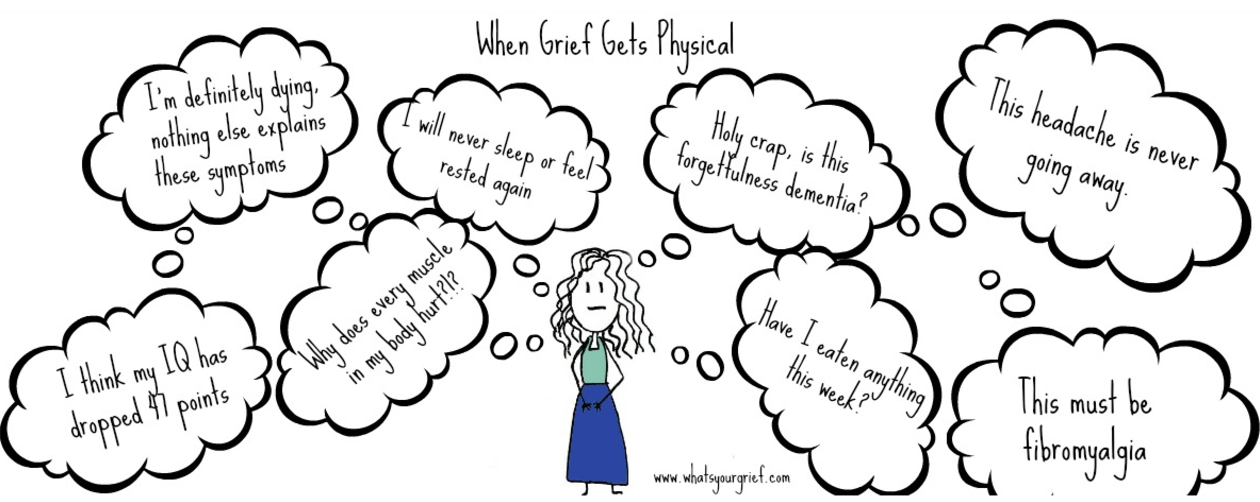
The death of a parent, caregiver or sibling has been found to be one of the most stressful life events that a child or youth can experience. Therefore it is important to provide children with information about grief, normalize their responses and encourage them to share their thoughts and feelings.
Children are often the hidden mourners in our society with little attention being paid to their bereavement needs. Every child has different needs, perspectives and understandings of what death means. Therefore it is important to provide children with information and education on death and grief as well as normalize their responses and encourage them to share their thoughts and feelings.
It is challenging to parent a grieving child when parents are themselves grieving. Grief is often isolating and consuming. Having access to resources and supports can help families feel connected and equipped to face their grief together.
Visit The Canadian Alliance for Children's Grief (CACG) for more information or resources. CACG is the first Canadian national group of professionals working together to ensure the accessibility of bereavement support and information to grieving children, teens and their families. Resulting from a collaborative effort amongst agencies and service providers across the country, the CACG seeks to address the barriers experienced by organizations providing services to grieving children and youth and strengthen the support offered to local communities. Source: CACG