The links to the podcasts of Death: A Part of Life are listed below:
Death, A Part Of Life - Part 1: Palliative Care.
It’s a fact of life that at one point we all will die. But is it all as simple as that? Bill Kelly and the Bob Kemp hospice will be discussing grief, relief and the acceptance of passing away. On today’s show we discuss what happens when you’re told you don’t have much time left, and whether healthcare is asking too much of caregivers, and whether people are prepared for palliative care.
Death, A Part Of Life - Part 2: Changes To Palliative Care.
For our second show, we will discuss what the palliative care system is now, how it works and what changes need to be made. What does one of our local MPPs hear from his constituents about healthcare and in particular, palliative care? How would changes affect patients? Does fear have a hold on how we make our decisions once we’re diagnosed as palliative? An example of this is whether to choose palliative care or medically assisted death.
Death, A Part Of Life - Part 3: Religion and Palliative Care.
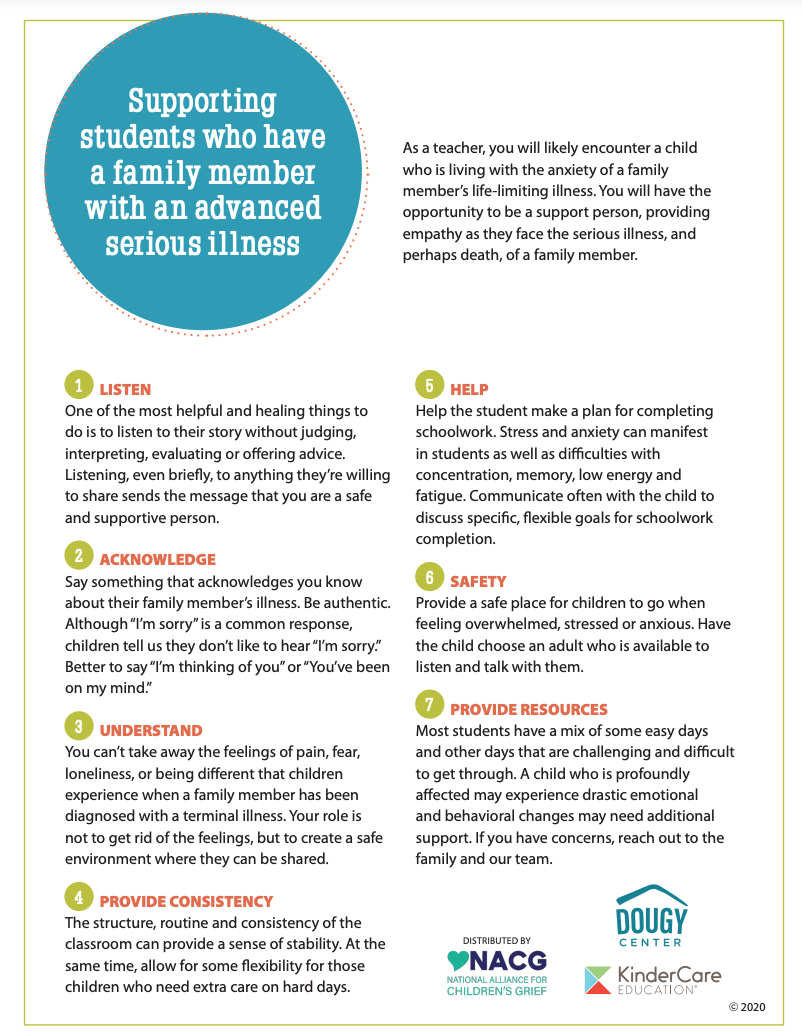
We continue our series this week with two topics. The first one will be discussing the experience of death. Everyone treats death in our world differently. But is it strictly a medical experience or is it a spiritual one? In our second half, we will talk about access to palliative care services in various sectors of our society. How do we help the vulnerable and the community obtain access to proper palliative care?
Death: A Part of Life - Part 4: Bucket lists and preparation.
Life should be celebrated at all stages, whether it be infancy, adulthood and as life comes to a close. So how can we make the most out of life? How can those who are in palliative care achieve their “bucket list” dreams before they pass, and how does it apply when it comes to their own personal circumstances? How do we define a “bucket list”? How wise is it to be prepared for eventual health issues? How should we plan for advanced care and how does it affect the family? How do we navigate through the difficult decisions and pain to provide care for loved ones who are palliative?
Death: A Part of Life - Part 5: The grieving process.
The final instalment in our series sees us discussing grief and how this isn’t just an event that happens in life but a process that families have to go through. How do families grieve the loss of a loved one? How can we support one another and how does grief affect children?
Source: Global News. AM 900 CHML