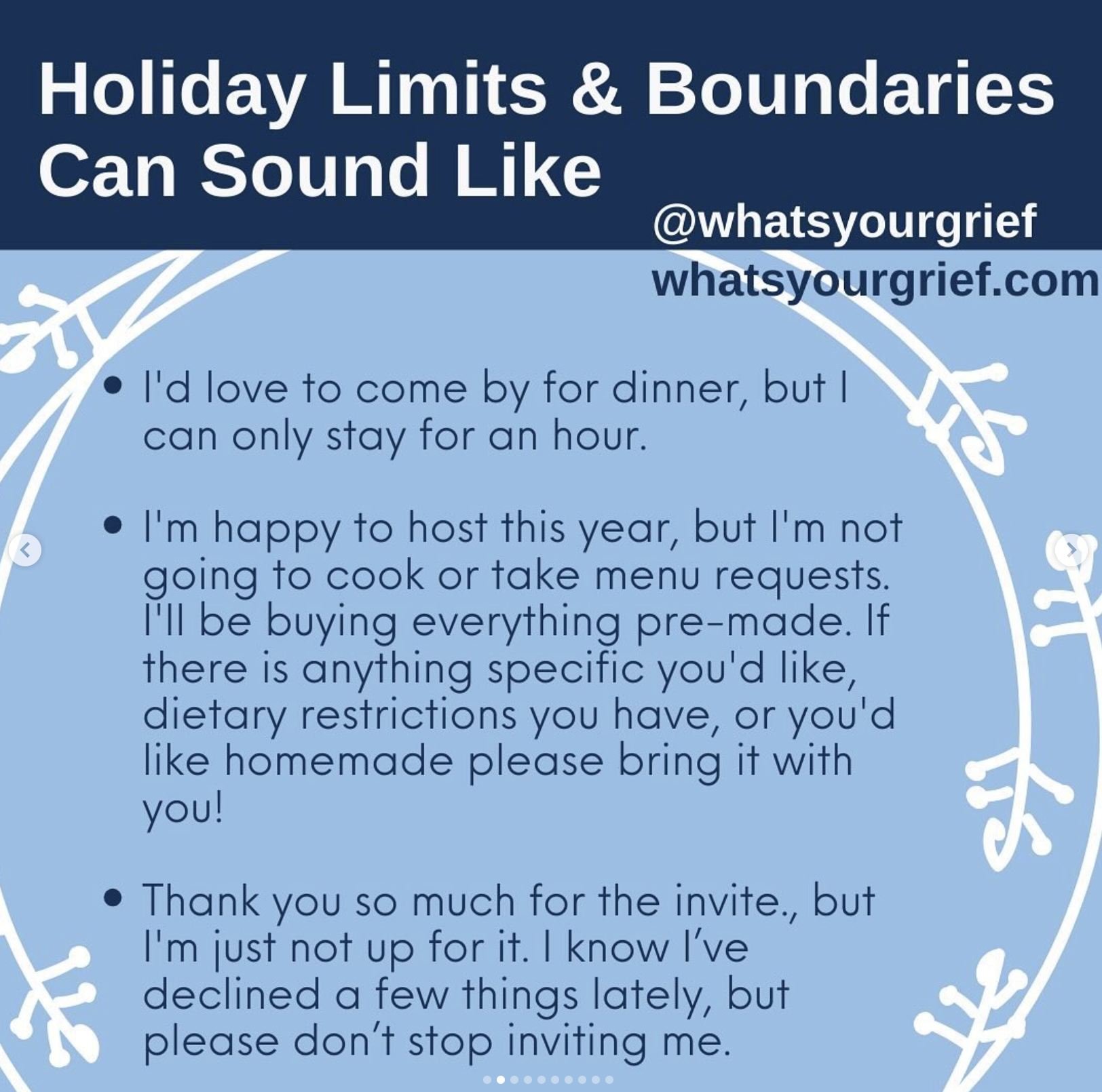
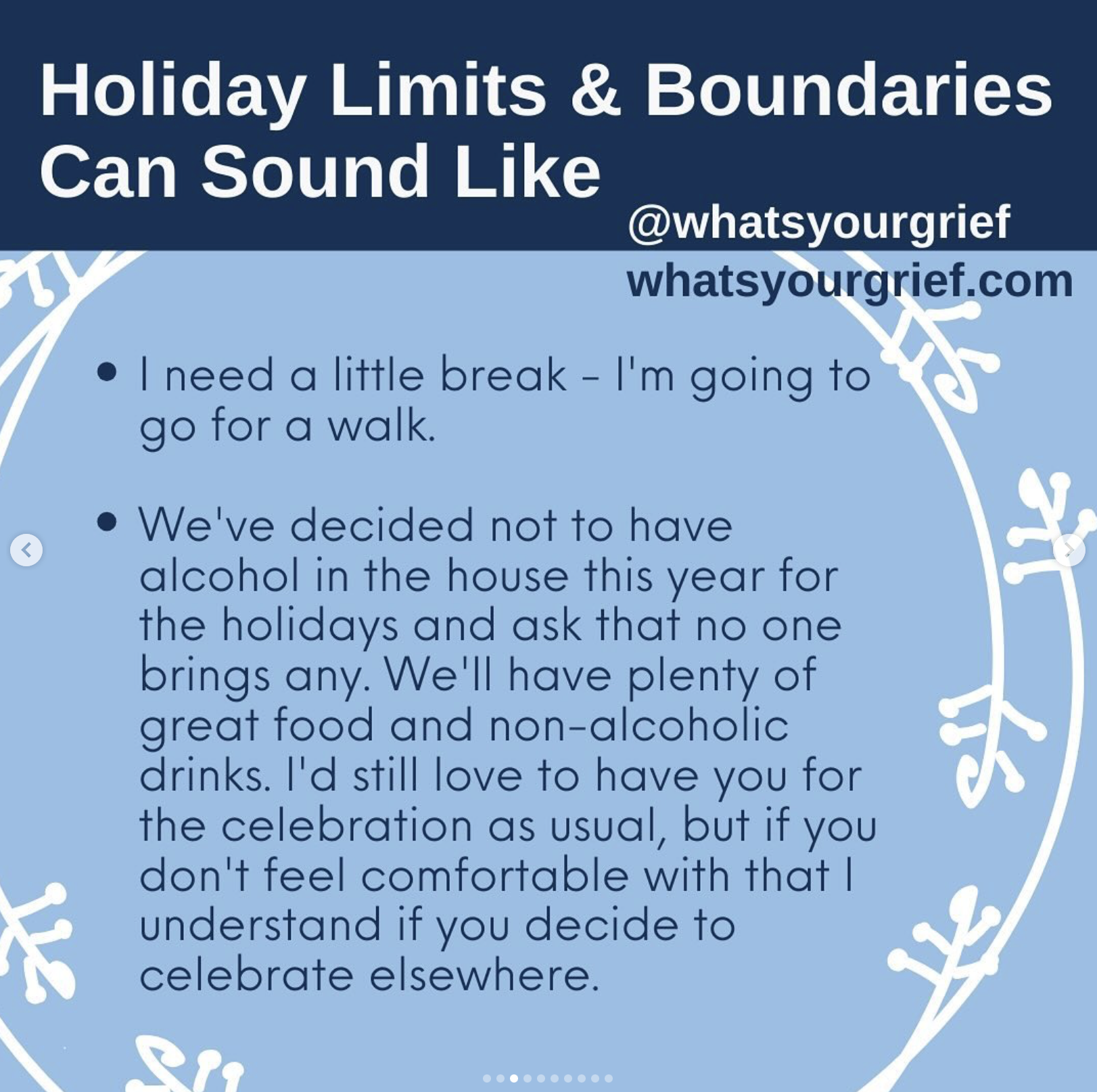
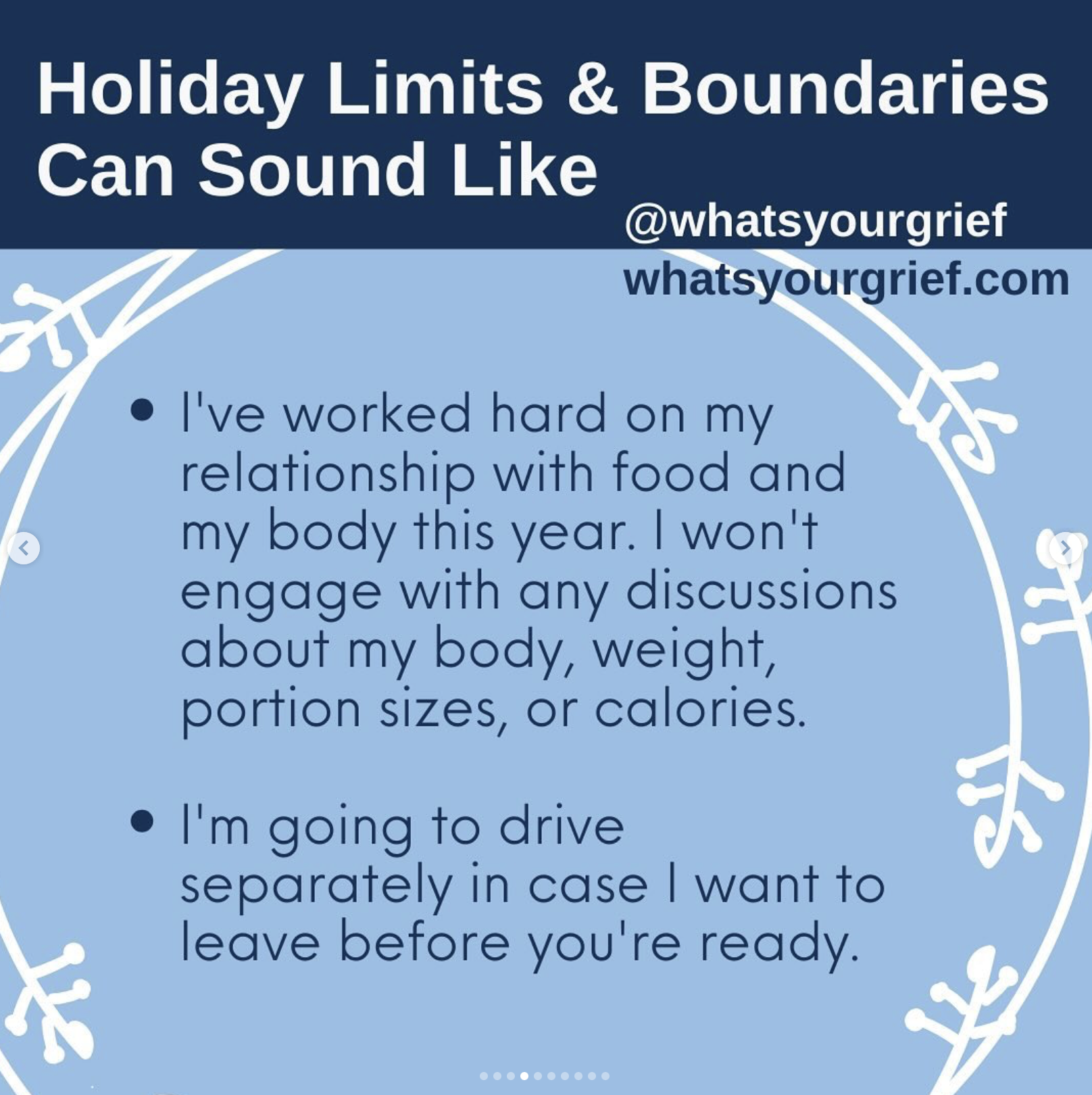
Holiday Limits, Boundaries and Self-Compassion Reminders" via What’s Your Grief (WYG). Visit Archive for the Holiday Season via WYG
How to Survive The Holidays When You're Grieving
How to Survive The Holidays When You're Grieving via Megan Devine
"The holiday seasons adds an extra measure of pain to people already bearing more than they can, more than they should ever have to. There is the empty seat at the table, the heaviness of all the ways the one you love is missing, traditions that have gone flat, smacking against the empty place.
Death, illness, massive life events — they all sour the season in ways those outside your loss can’t understand. Given that this season is going to be rough, how will you survive? Here are some of my holiday survival rules from my own early days. Remember, whatever you choose to do (or not do) this holiday season, staying true to yourself is important.
If you have someone who consistently tries to talk you out of your 'no,' you might respond by calling them out on their coercion: 'I keep telling you no, and you keep trying to convince me that I’m wrong. I need you to respect my decision.' Friends and family get to feel disappointed in your no, but they don’t get to force you to say yes.
Whether you are missing someone who should be part of the festivities, or you are missing someone who shared your love of quiet acknowledgment over raucous partying, this season will likely add to your grief.
Companion yourself. Care for yourself. Listen to yourself. Reach out where it feels good to reach, curl in when that is what you need. Make this season as much of a comfort to yourself as you can.
May your holiday season (or non-holiday, depending) be as safe, and full of love and connection as it can be.”
Visit refugeingrief.com for more Grief Support.
Grief & the Holidays: 6 Things to Remember
In the midst of the focus on joy & cheerful celebrations at this time of year, sharing a reminder of "Grief & the Holidays: 6 Things to Remember" via Claire Bidwell Smith
Children's Grief Awareness Day is observed on the third Thursday in November
Children's Grief Awareness Day is observed on the third Thursday in November. This time of year is a particularly appropriate time to support grieving children and youth as the holiday season is often an especially difficult time after a death.
Children's Grief Awareness Day brings attention to the fact that support can make all the difference in the life of a grieving child or teen. It provides an opportunity to raise awareness of the painful impact that the death of a loved one, with an opportunity to make sure that grieving children and teens receive support they need.
Children and youth who have experienced the death of someone important to them often feel isolated, like their struggles are invisible to those around them. Grieving children and teens need advocates and allies navigating supportive ways to move forward. Every school and community has children and teens who have experienced loss. Children’s Grief Awareness Day is about recognizing that no young person should have to navigate grief alone.
We raise awareness so that people will understand that a grieving child or teen can't just "get over it”, not in any set time period, not by any act of their own will - and that there's no reason they should just "get over it. We can ensure children and youth feel seen, heard, and understood with the right tools, compassion and support.
Source: Children's Grief Awareness Day
National Grief & Bereavement Day is November 19th
Remember. Reflect. Connect. National Grief and Bereavement Day is November 19, 2024. It is time to reflect and take action, creating connections while navigating grief.
The third Tuesday in November marks the annual National Grief and Bereavement Day in Canada. On this day, CHPCA encourages Canadians to engage government and all sectors of Canadian society in a national dialogue to identify and support access to the necessary resources for those living with grief and bereavement.
Grief can make us hesitant to connect with those around us, whether we are the person grieving or someone around them. When someone we know is faced with grief, we can often find ourselves at a loss for words. When we are grieving ourselves, we may not know what support we need.
Grief is Universal. Grief is a common experience we will all share, yet it can often leave us feeling disconnected. We might feel disconnected from our loved ones, from our friends, or from who we used to be.
Finding connection through loss can be a powerful tool to help us move forward and through grief. Something as simple as a phone call, someone reaching out, a hug, a prayer, or a treasured memory shared can bring much needed solace after a loss.
For more information, or to access a Grief and Bereavement Resource Repository, visit: https://www.chpca.ca/awareness/national-grief-and-bereavement-day/grief-and-bereavement-resource-repository/
Source: CHPCA
Demystifying Palliative Care: Exploring a Wrap-Around Approach to Quality of Life
Thank you to Wellspring Niagara for the invitation to present “Demystifying Palliative Care: Exploring a Wrap-Around Approach to Quality of Life”.
It is important to acknowledge the barriers exist - to education, services, funding & resources.
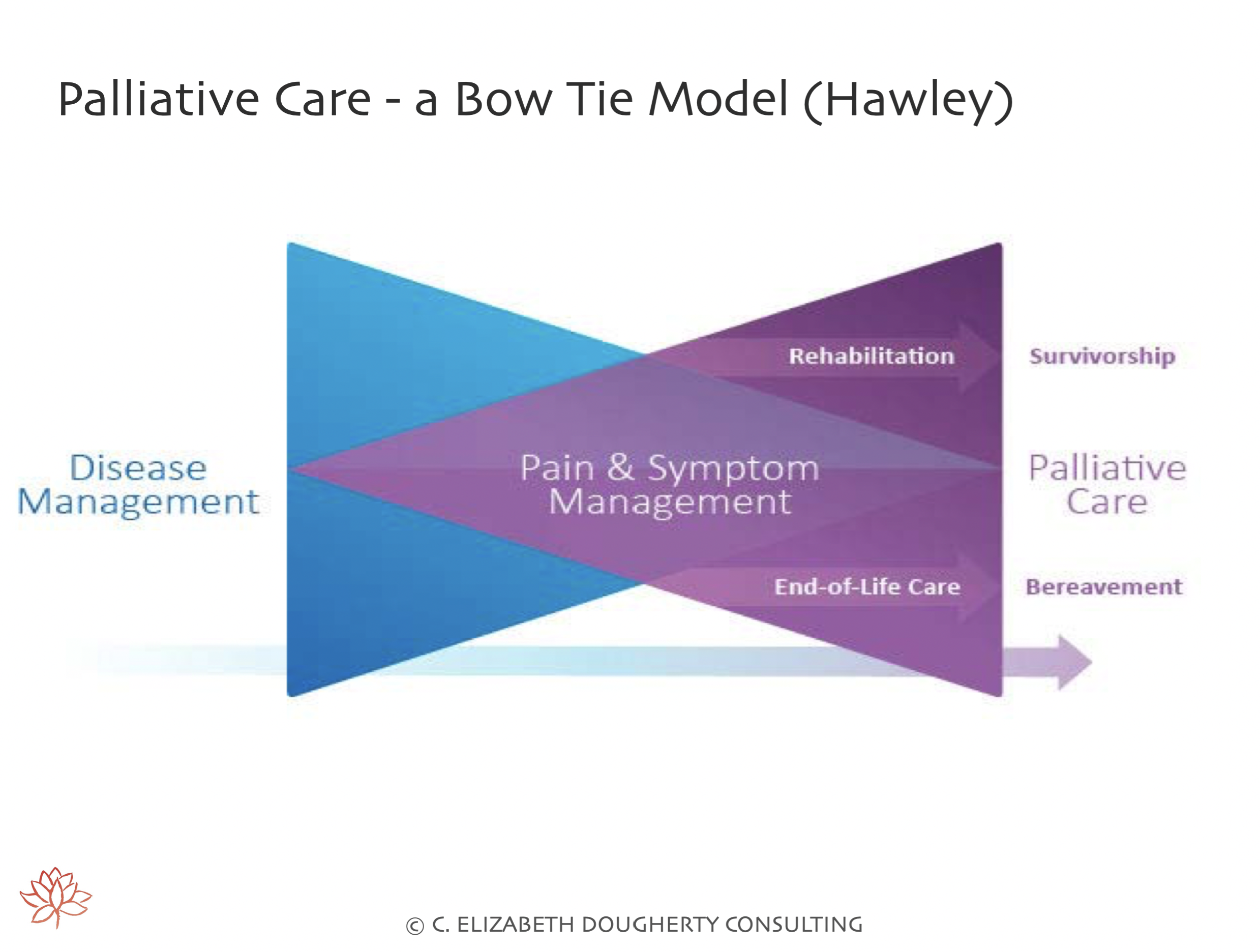
Did you know that Palliative Care is:
Appropriate for any person & or family living with, or at risk of developing, a complex illness due to any diagnosis, with any prognosis, regardless of age, & at any time they have unmet expectations & or needs, and are prepared to accept care
May complement & enhance disease-modifying therapy, OR it may become the total focus of care
Most effectively delivered by an interprofessional team who are both knowledgeable & skilled in all aspects of the caring process related to their discipline
Treats all active issues & prevents new issues from occurring
Addresses physical, psychological, social, spiritual and practical issues, & their associated expectations, needs, hopes & fears
Prepares for & addresses self-determined life closure & the dying process;
Assists in coping with loss & grief throughout the illness & into bereavement
Yet SO many barriers exist, including:
Few Canadians (15%) have EARLY access to Palliative Care
Palliative Care provided during admission to hospital was unplanned or through an emergency department 80% of the time
62% of Canadians who received Palliative Care did so in an acute care hospital in their LAST month of life
Palliative Care is a patchwork of uncoordinated services
Palliative & end-of-life care remain underfunded - receiving only ~1% of the overall investment in cancer research
Mandatory education should be required for ALL healthcare providers due to the team-based nature of high-quality palliative care, including culturally safe palliative care, grief & bereavement supports
Structurally vulnerable & marginalized communities including: Unhoused people, Indigenous communities, non-English speaking patients, young patients & 2SLGBTQ+ individuals & families face additional barriers to care resulting in inequitable access.
It is essential that we address barriers and stigma surrounding Palliative Care as this impacts access to care - for anyone facing a complex illness (curative or life-limiting).
World Hospice and Palliative Care Day is Saturday October 12th
Palliative Care is often misunderstood.
10 Myths About Palliative Care infographic dispels common misconceptions about palliative care.
This resource is available in English and 13 other languages, including:
-French
-Arabic
-Brazilian Portuguese
-Catalan
-Chinese
-Cree
-Hebrew
-Inuinnaqtun
-Japanese
-Portuguese
-Spanish
-Tagalog
-Kinyarwanda
Download and share the infographic in your preferred language via:
https://www.virtualhospice.ca/en_US/Main+Site+Navigation/Home/Support/Resources/Books_+Links_+and+More/
Source: Canadian Virtual Hospice
World Hospice and Palliative Care Day is Saturday October 12th.
“We believe that it takes a society to create better treatments, better care, and better support for people living in Canada. Part of making further advancements is offering recommendations to federal and provincial governments that can make supports for people with cancer more accessible, like palliative care.” Source: CCS
The Canadian Cancer Society’s (CCS) report analyzing palliative care across Canada will direct advocacy and support initiatives in the coming years. This report highlights 4 key findings about palliative care:
1. Canada still lacks the capacity to consistently deliver palliative care in communities, particularly in hospice.
2. There are significant social barriers to talking about death and dying, and confusion about the benefits of palliative care.
3. All provinces and territories noted that more could be done to improve cultural safety in palliative care, including grief and bereavement supports.
4. Access to palliative care would be enhanced with additional training of healthcare professionals in more healthcare settings.
To ensure that palliative care reaches those who require it, there needs to be a shift in the awareness and understanding of services for everyone, including providers, caregivers, and patients. There also needs to be an increased understanding of the landscape of palliative care services across Canada. The palliative care needs of a population cannot be met by palliative care specialists alone.
Source: 4 key findings about palliative care. CCS
To read more, visit: https://cancer.ca/en/about-us/stories/2024/4-key-findings-about-palliative-care
World Hospice and Palliative Care Day is Saturday October 12th.
This is an annual unified day of action to celebrate and support hospice and palliative care around the world and the theme this year is: Ten Years Since the Resolution: How are we doing? The year 2024 marks 10 years since the World Health Assembly (WHO’s Governing Body) passed the only stand-alone resolution on palliative care, calling for all countries to “strengthen palliative care as a component of comprehensive care throughout the life course.”
Palliative care is recognised as a fundamental component of health care systems, including Universal Health Coverage and primary health care. Yet, sadly, approximately 86% of people around the world who need palliative care cannot access it. Some 18 million people die every year with pain and suffering, due to lack of access. Much of the problem of lack of care is caused by a lack of awareness of how palliative care should be given, and why it is important.
On this World Hospice and Palliative Care Day, we call upon governments, policymakers and providers to prioritise and implement national strategies for bereaved populations based on a public health approach. It is estimated that for each death, up to 9 people are directly affected by the loss. Given that about 120 million people died over the past two years (including over 6 million from COVID), Then over a billion people are experiencing bereavement by one or more deaths of people significant to them in the past two years.
If you would like any further information, please visit the World Hospice and Palliative Care Day website for more information about events at http://www.thewhpca.org/world-hospice-and-palliative-care-day.
Source: The THE WORLDWIDE HOSPICE PALLIATIVE CARE ALLIANCE
National Children’s Hospice Palliative Care Day is Thursday October 10th.
"National Children’s Hospice Palliative Care Day raises awareness about the importance of children’s hospice palliative care and how it improves the quality of living and dying for children with serious illnesses and their families. The campaign is co-hosted by CHPCA and the Canadian Network of Palliative Care for Children (CNPCC), every year on the second Thursday of October." Source: Canadian Hospice Palliative Care Association CHPCA
"Every child and teen deserves a full, happy life filled with love. How can we make sure that happens for children with a serious illness? That’s where children’s hospice palliative care teams come in. The focus of Pediatric Palliative Care is on improving the quality of life of the child and their family. That means support for:
Symptom management
Emotional and spiritual needs
Building connections with other children and families on similar journeys
Making memories and finding joy as a family
And so much more!
Pediatric Palliative Care teams are there to lighten the load, to walk alongside families on this journey, and to give them the support and resources they need so they can focus on the little joys and precious moments together.
This day is a call to action. It’s time to recognize that children’s hospice palliative care is not just a specialty. It is a shared responsibility across healthcare and communities to help children and families Make Every Day Count.” Source: CHPCA
To learn more, visit National Children’s Hospice Palliative Care Day. Canadian Hospice Palliative Care Association (CHPCA)
National Children’s Hospice Palliative Care Day is Thursday October 10th.
"The main goal of palliative care is quality of life, including relief from symptoms of physical and emotional illness and stress. Palliative care is appropriate for any child that has received a serious diagnosis or for whom the prognoses has become serious. The PPC team helps to coordinate your child’s care and can act as a liaison between you and the care team (and, really, everyone in your life who is involved with this illness journey)." Source: Courageous Parents Network (CPN)
"Pediatric palliative care providers can help with a whole host of challenges that may arise during a child’s cancer treatment. It isn’t just symptom management. This can include navigating difficult conversations and serving as an interpreter for the child." Source: Courageous Parents Network (CPN)
"What if" conversations are hard. However, having them with your clinicians can help you find the anticipatory guidance you crave and help you better define your goals of care for your child. Understand more about goals of care by visiting the CPN website". Source: Courageous Parents Network (CPN)
Watch Dr. Toluwalase Ajayi, a Pediatric Palliative Care physician explain the "PERSON Model" to explore what parents/caregivers are wondering for their child:
Perception
Explore
Relate
Sources of Worry
Outlining Next Steps
Notify
via Courageous Parents Network (CPN) https://courageousparentsnetwork.org/videos/a-palliative-care-md-on-the-person-model-for-assessing-peoples-goals-of-care
To learn more about Palliative Care and how can help, visit CPN at https://courageousparentsnetwork.org/topics/how-palliative-care-helps:
Visit the incredible FREE resource - The Courageous Parents Network (CPN) mobile APP - a quick and easy way for families caring for very sick children, and the providers who support them, to find, save, carry and share Courageous Parents Network (CPN) content (videos, podcasts, guides and more resources) and register for free CPN events.
Demystifying Grief and Honouring Loss: Exploring Healing While Caring For Others And Ourselves
I am honoured to once again deliver the UGME lecture “Demystifying Grief and Honouring Loss: Exploring Healing While Caring For Others And Ourselves” to the Michael G. DeGroote School of Medicine at McMaster University.
Grief is simply one word that cannot begin to describe a universal, yet uniquely complex and deeply personal, series of life-changing events and losses while still finding ways forward.
Acute care hospitals focus on short-term episodic care & interventions and treatments aimed at cure, creating an environment where death is seen as a failure, or where death is denied. What does this mean when dying and death are inevitable?
It is so essential in whole person and *family-centred care, that we explore impact on the person and family, not just treat part of the body, or acknowledge a fraction of the medical event, or illness. This is true for all we serve, and this is also true for healthcare providers stepping forward to deliver care who are deserving of care and support for themselves.
What does it mean to explore and honour grief for anyone facing trauma and loss stemming from acute medical events, complex illness, dying, death, bereavement - for any person and family, AND the healthcare providers caring for them?
A reminder, while largely stigmatized and misunderstood, in the words of Dr. Kenneth Doka,
“Grief is a reaction to loss. We often confuse it as a reaction to death. It’s really just a very natural reaction to loss. When we lose any significant form of attachment, grief is the process of adjusting”
Grief is a process, a uniquely personal ongoing process.
Grief can fracture one’s entire world, temporarily, or permanently.
Following an acute medical event, or a diagnosis, grief can fracture identities, hopes, routines, connections, sense of control and safety. Grief, largely invisible to others, is incredibly isolating, leaving the individual to navigate a fractured world, often alone – even when surrounded by others.
Modern medicine focuses on cure and fixing. In grief, healing focuses on care and process.
Learn to sit with (OR move with) grief as this demonstrates a sense of presence that is open, engaged and compassionate with the process of metabolizing grief, and in doing so, honours the losses, and the connections.
*family is always best defined by the individual we serve, as family, and loss of connections to family, are others sources of trauma and loss.
FREE Death Café: Wednesday August 7th (6-8pm)
I am honoured to co-facilitate a FREE Death Café at the David Braley Health Sciences Centre, together with Dr. Alan Taniguchi, McMaster University on behalf of The 100% Certainty Project. Death: Something to Talk About and The Division of Palliative Care.
Registration is required for this FREE Death Café on Wednesday August 7th (6-8pm) via Eventbrite at: https://www.eventbrite.ca/e/death-cafe-tickets-914115994547?aff=oddtdtcreator
Death Café is an international movement where people, often strangers, gather to eat, drink tea and discuss death. The objective is 'to increase awareness of death with a view to helping people make the most of their (finite) lives’.
At Death Café, you can expect a group directed discussion of death with no agenda, objectives or themes. It is a discussion group.
Please note that Death Café is NOT a grief support group, nor is this a grief counselling session.
Death Café is a respectful, public event where people of all communities and belief systems are welcome to have respectful discussions about death.
Interesting conversation is guaranteed! For more information about Death Café, please visit https://deathcafe.com/
Image via YG2D For more information on YG2D visit https://www.yg2d.com/
Image via YG2D For more information on YG2D visit https://www.yg2d.com/
Proud, Prepared, and Protected
“Proud, Prepared, and Protected is a collection of online FREE resources to assist people who identify as 2SLGBTQ+ to access and receive inclusive, respectful care. These resources were developed by people who identify as Two-Spirit and LGBTQ+ and more than 40 organizations and Canadian Virtual Hospice to fill a national gap. This information is also helpful for allies, people working in healthcare and education and communities.” Source: Canadian Virtual Hospice
To access free resources, visit: Proud, Prepared, and Protected
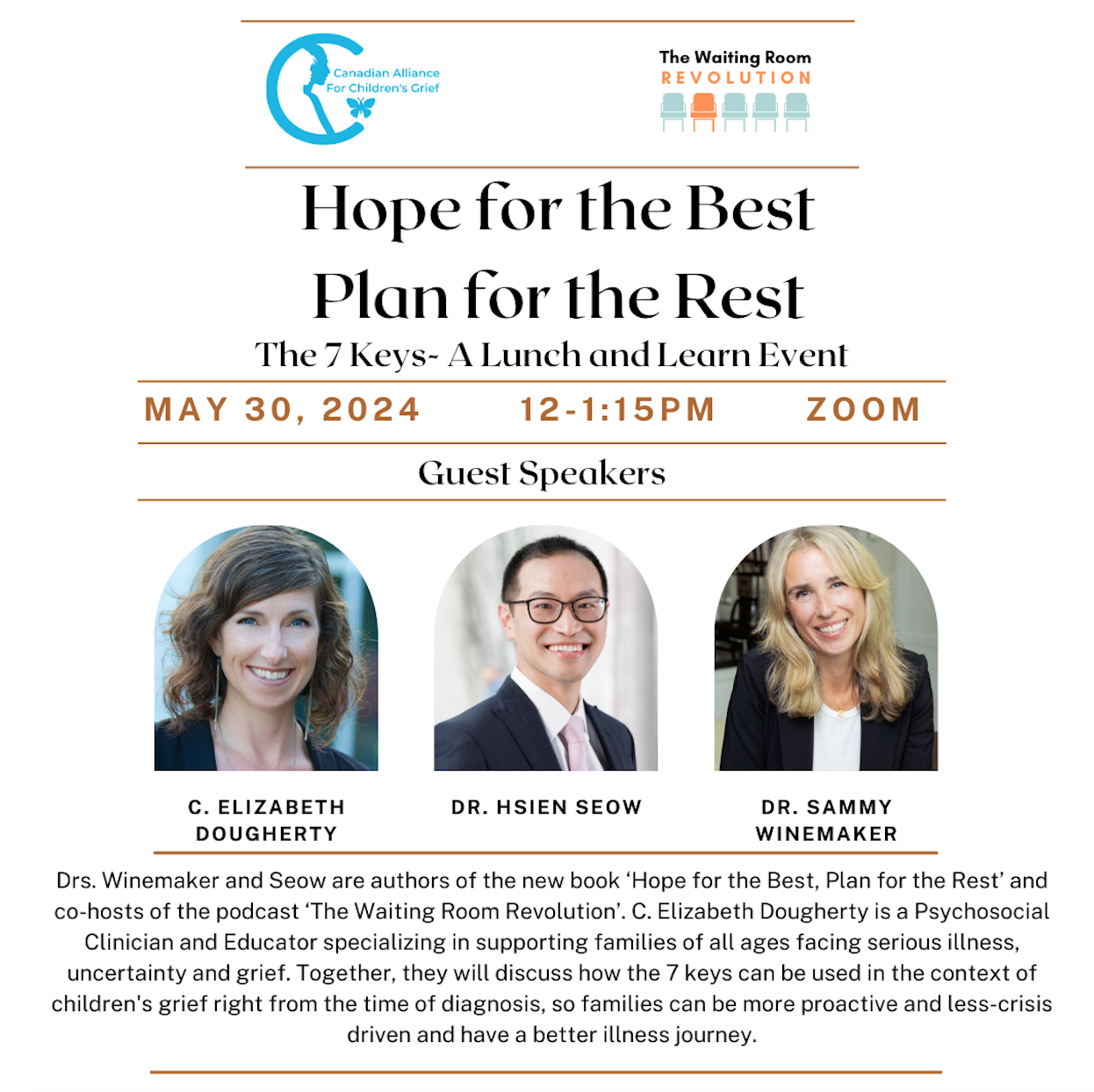
Hope for the Best Plan for the Rest The 7 Keys - A Lunch and Learn Event
I am thrilled to be in conversation with fabulous colleagues from McMaster University, Dr. Hsien Seow & Sammy Winemaker of The Waiting Room Revolution.
Dr.'s Seow and Winemaker are extraordinary advocates and brilliant communicators focused on supporting individuals, families and communities navigating serious illnesses and facilitating empowered experiences within the healthcare system.
"Hsien and Sammy have spent their careers helping those who are facing serious illness. For years, they often heard patients and families say they felt unprepared and overwhelmed. Despite years of education, research, and advocacy, they continued to hear patients and families say 'Why didn’t anyone tell me that sooner…'
They started the Waiting Room Revolution movement because they wanted to improve the patient and family illness experience. They want to build a community to share deeply human stories about caring for others. Through interviews with experts, clinicians, patients and caregivers, they are harnessing the advice of those with lived experience to better prepare those who are just starting their caring journey." Source: The Waiting Room Revolution
Join us for Hope for the Best Plan for the Rest The 7 Keys - A Lunch and Learn Event with the Canadian Alliance for Children’s Grief via ZOOM
Guest Speakers:
Drs. Winemaker and Seow are authors of the new book ‘Hope for the Best, Plan for the Rest’ and co-hosts of the podcast ‘The Waiting Room Revolution’. C. Elizabeth Dougherty is a Psychosocial Clinician and Educator specializing in supporting families of all ages facing serious illness, uncertainty and grief.
Together, they will discuss how the 7 keys can be used in the context of children's grief right from the time of diagnosis, so families can be more proactive and less-crisis driven and have a better illness journey.
Please register via this link.
Source: The Waiting Room Revolution
The essential guide for every patient and family diagnosed with a life-changing illness
"The essential guide for every patient and family.
When you are diagnosed with a life-changing illness, it can be overwhelming. While your diagnosis cannot be changed, the way you experience your illness can.
In Hope for the Best, Plan for the Rest, we draw on our decades spent researching and caring for thousands of seriously ill patients to reveal the seven keys for a better illness experience. With real-life stories, tips, and exercises to improve your journey right from diagnosis, we want to empower you with practical tools to navigate the healthcare system with knowledge, confidence, and clarity.
You can find hope in the face of uncertainty. You can live well, be fully informed, and be activated - and feel more like a person and less like a patient. But most of all, you can be hopeful and prepared at every step along the way."
Source: Waiting Room Revolution
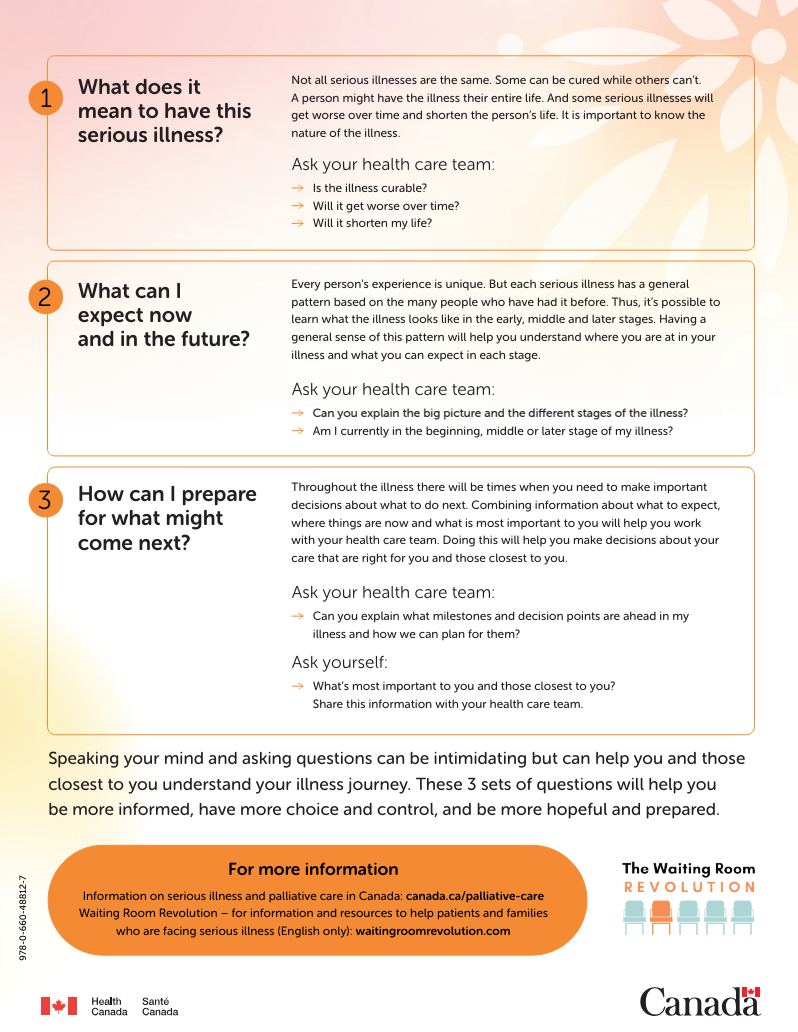
What to do when facing a serious illness
What to do when facing a serious illness: 3 sets of questions to ask your health care team
Receiving a diagnosis of a serious illness can be overwhelming. Often people don’t know what the journey will look like. However, there are things you can do to help you communicate with your healthcare team. For example, you and those closest to you can ask key questions to make sure you understand your illness.
1. What does it mean to have this serious illness?
2. What can I expect now and in the future?
3. How can I prepare for what might come next?
For more information:
On Serious Illness and Palliative Care in Canada: canada.ca/palliative-care
Waiting Room Revolution for information and resources to help patients and families who are facing serious illness (English only): waitingroomrevolution.com
Source: @waitingroomrev
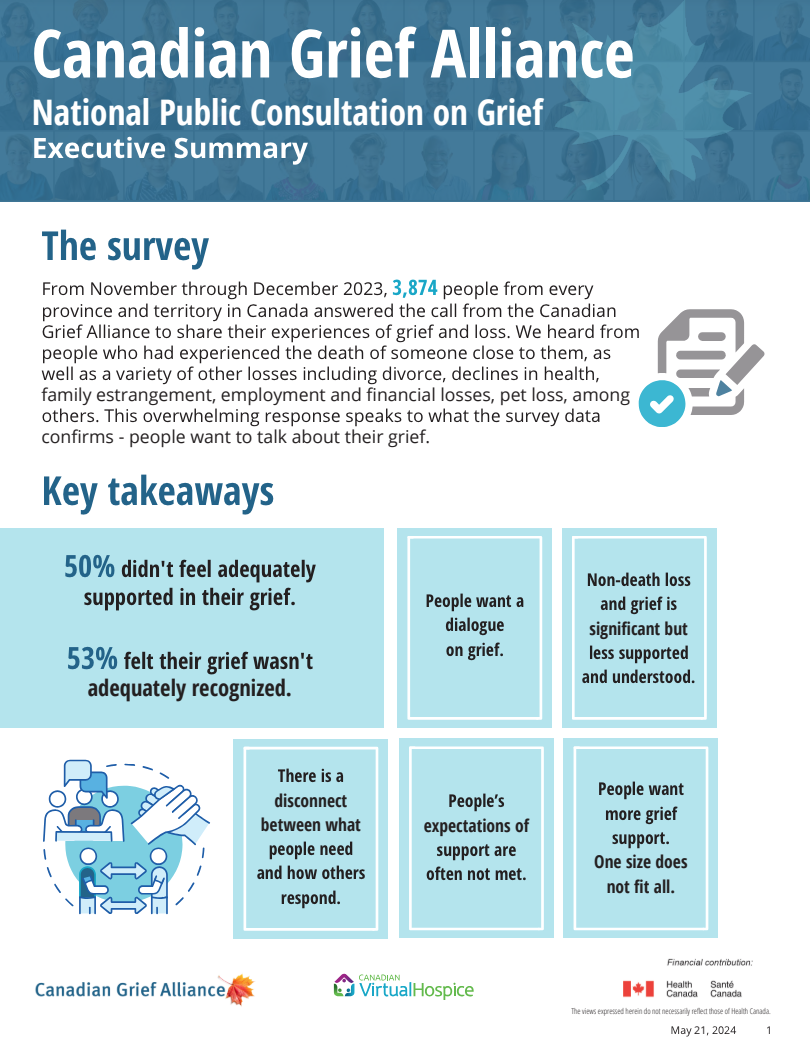
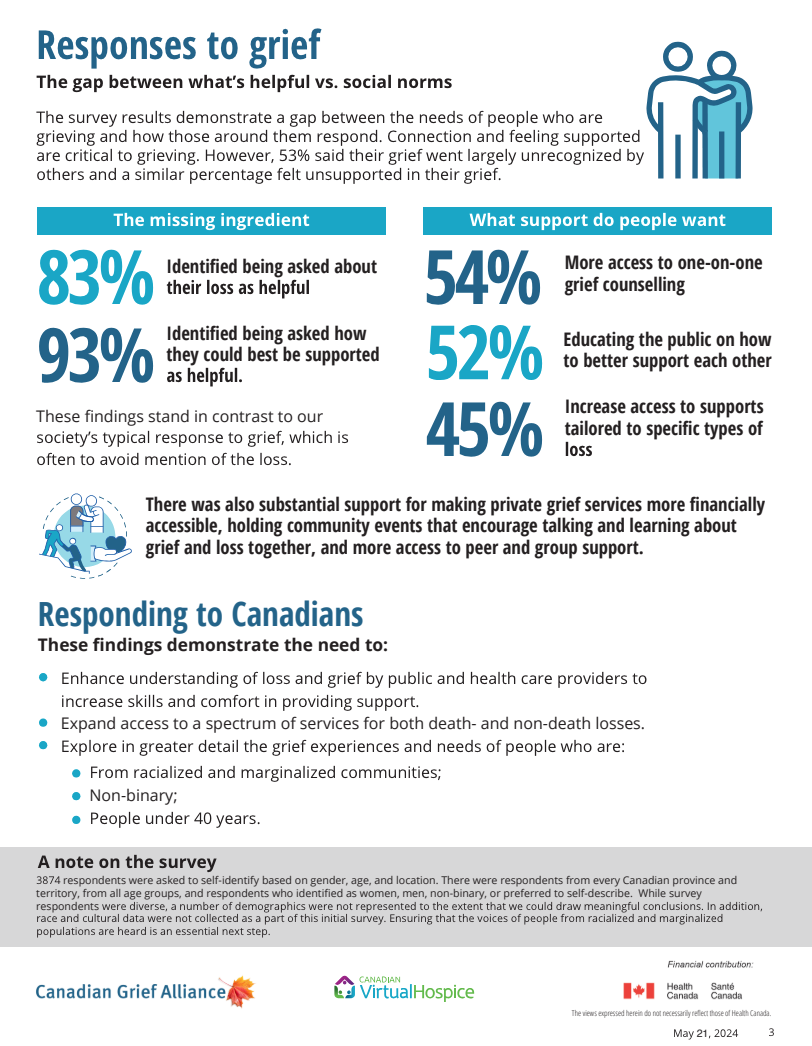
The largest ever survey on grief in Canada has been released...
The largest ever survey on grief in Canada has been completed and results have been published, though sadly, not surprising...
"Results from the largest grief survey ever conducted in Canada show that the very thing that many people want most when they are grieving - to be asked about their loss - is not how society is likely to respond.
The Canadian Grief Alliance (CGA), Canadian Virtual Hospice has released the findings of its landmark public survey on grief. With nearly 4,000 respondents, the survey is the largest ever on grief in Canada and will inform a National Action Plan for Grief which the CGA will present to the federal government in 2025.
Key findings include:
- 53% of respondents said their grief went largely unrecognized by others
- 50% of respondents felt inadequately supported in their grief
- 83% of respondents identified being asked about their loss as being helpful
- 54% of respondents wanted more access to one-on-one grief counselling
- 52% of respondents thought educating the public on how to better support each other would be helpful
Survey results point to the need to:
- Enhance understanding of loss, grief, and how to provide support among the public and professionals
- Expand access to a spectrum of grief services for both death- and non-death losses.
-Explore in greater detail the grief experiences and needs of people who are: from racialized and marginalized communities; Non-binary; Under age 40".
Source: CGA and Canadian Virtual Hospice
To read more, please visit: CGA Executive Summary
Holding Exquisite Presence When Supporting Children and Their Families Who are Grieving
I was incredibly honoured to join my compassionate friend and dear colleague, Rami Shami, in a creative space, talking about the need for grief to come out of the shadows.
“How we support children and youth in their grief can have a lasting impact on their mental, emotional, even physical health. Joining us on this podcast is an individual who draws on her knowledge and experiences as an educator, a clinician in private practice, and a mother, in sharing how to hold what she calls, 'exquisite presence,' when supporting children and youth who are grieving. Her approach, garnered through decades of in the field work within numerous settings, highlights practical and informative insights into the disenfranchisement of grief amongst children, and how promoting safe spaces can help children process their experiences of loss. Join us for an exceptional informative and educational podcast!”
Source: The Lighthouse Beacon Podcast
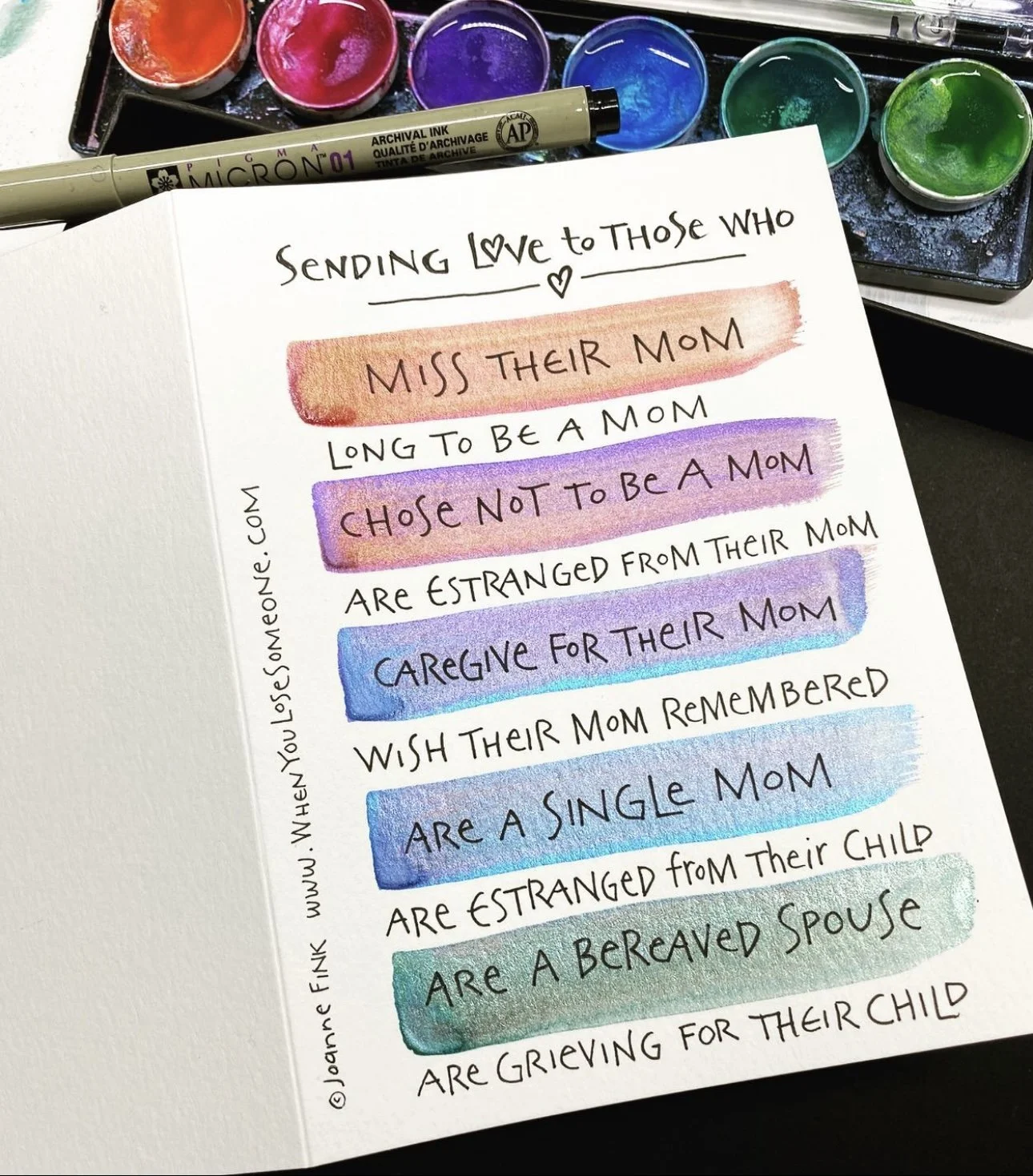
On Mother's Day...
Thinking of everyone on Mother's Day, in a multitude of ways... for all this day means for you, and for all that it holds, sending love and light.
Wishing grace and peace. ❤️