This enactment provides for the development and implementation of a framework designed to guarantee all Canadians access to high-quality palliative care.
1. This Act may be cited as the Framework on Palliative Care in Canada Act.
Development and implementation
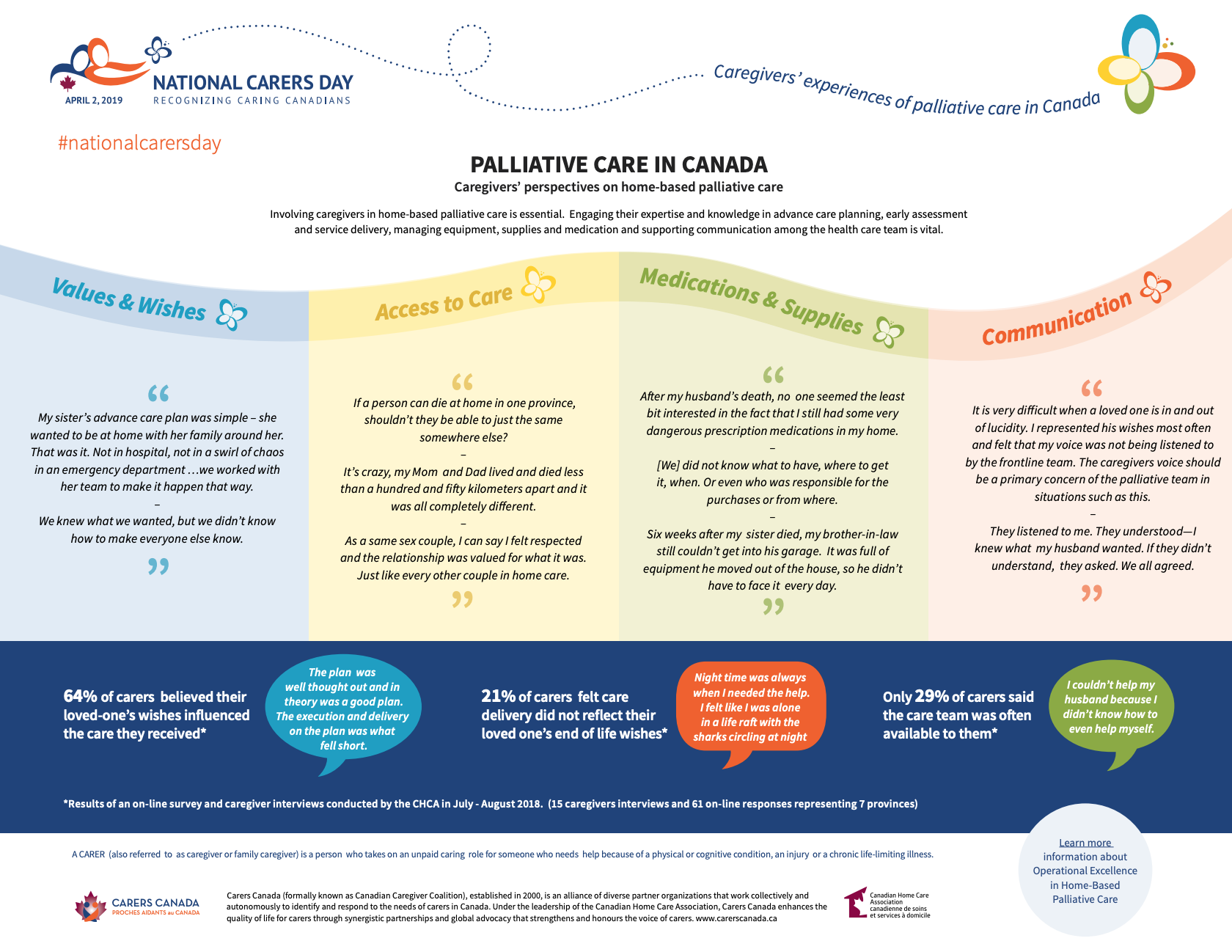
2. (1) The Minister of Health must, in consultation with the representatives of the provincial and territorial governments responsible for health, as well as with palliative care providers, develop and implement a framework designed to give Canadians access to palliative care — provided through hospitals, home care, long-term care facilities and residential hospices — that, among other things,
(a) defines what palliative care is;
(b) identifies the palliative care training and education needs of palliative health care providers;
(c) identifies measures to support palliative caregivers;
(d) collects research and data on palliative care;
(e) identifies measures to facilitate a consistent access to palliative care across Canada; and
(f) evaluates the advisability of amending the Canada Health Actto include palliative care services provided through home care, long term care facilities and residential hospices.
Source: Parliament of Canada