How the fear of dying taught me how to live
"Live. Put your phone down. Talk to the person in front of you. Hold the door for people. Smile if someone catches your eye. Say thank you. Say please. Give hugs. Compliment people. Compliment yourself. Love yourself. No one will remember what size the pants are you are wearing but they will remember the way you walked in them. So walk softly. Speak boldly. Love gently. Laugh loudly. Call someone if they cross your mind. Allow yourself to be happy for others, and most importantly allow yourself to be happy for yourself, through every stage and step of your life. Be happy. Life doesn't have to be perfect for it to be perfect."
Unfinished Business in Families of Terminally Ill with Cancer Patients
" Families with unfinished business had significantly higher depression and grief scores after bereavement compared with those without."
Source: Unfinished Business in Families of Terminally Ill with Cancer Patients
10 Things My Chronic Illness Taught My Children
"All three of us work to maintain balance — knowing when we need to flex and when we need to release, when to put pain first and when to let it fade into the moment."
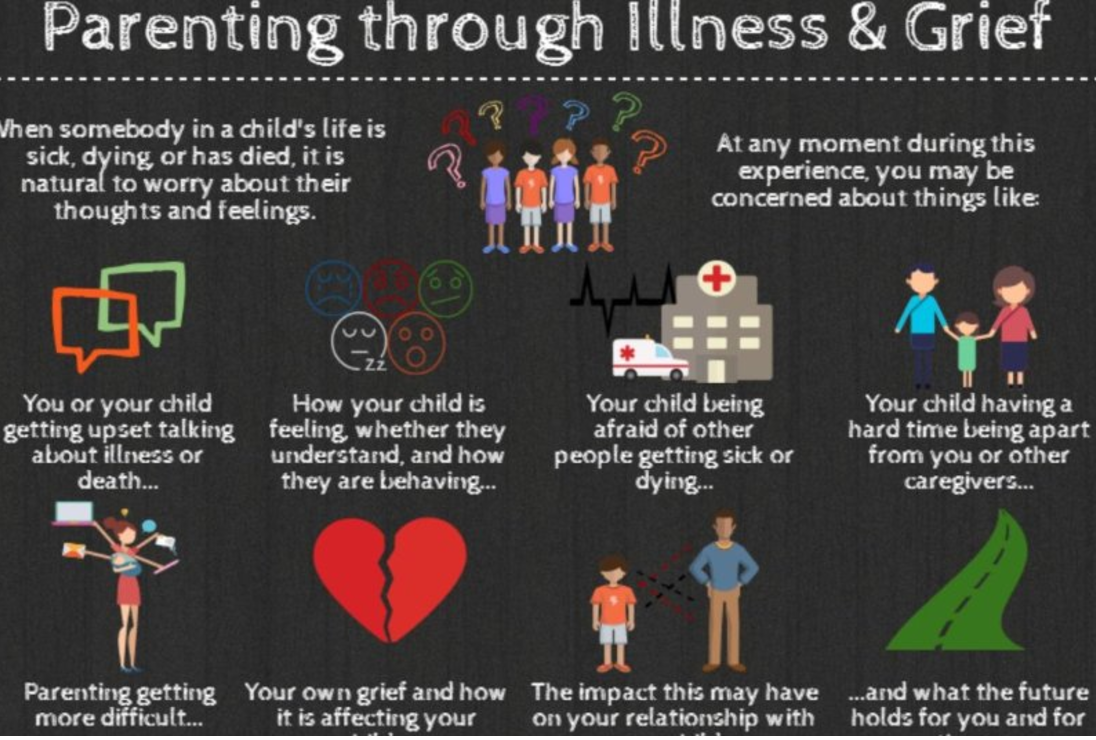
Parenting Through Illness & Grief
"This one page handout provides an overview of the findings from a research study of parent caregivers. The study was conducted as a collaboration between Dr. Jay Children`s Grief Centre and the Nanny Angel Network"
Source: Parenting Through Illness & Grief. Canadian Virtual Hospice
5 ways to improve care at the end of life
"All of us face the difficult prospect of a parent or loved one suffering from an illness that ultimately leads to death. When that time comes, we will want to ease their physical and emotional pain, respect their wishes, and allow them to die with dignity — the same things we will want for ourselves.
The way that Americans die has changed but, unfortunately, our medical system hasn’t kept up. It was designed at a time when death was often sudden or declines in health were relatively rapid. These days it is much more common for people to live longer with multiple chronic conditions, and we have the technology to prolong life as death approaches. End-of-life care is fragmented, intensive, and costly — and patients’ wishes are often lost due to poor communication."
Read the complete article at: STAT
LETTING GO: What should medicine do when it can’t save your life?
“People have concerns besides simply prolonging their lives. Surveys of patients with terminal illness find that their top priorities include, in addition to avoiding suffering, being with family, having the touch of others, being mentally aware, and not becoming a burden to others. Our system of technological medical care has utterly failed to meet these needs, and the cost of this failure is measured in far more than dollars. The hard question we face, then, is not how we can afford this system’s expense. It is how we can build a health-care system that will actually help dying patients achieve what’s most important to them at the end of their lives.”
An Innovative Approach to Family-Centred Legacy Projects
I am a Palliative Social Worker and for the past 17 years have had the privilege of caring for people facing a life-limiting illness. It is an intimate and profound experience - sitting alongside people as they face end-of-life. They share their hopes and fears - about living and dying - and about caring for and leaving behind those they love. Trying to protect their families while also wanting to prepare them. Grieving these losses begins at time of diagnosis.
I recognize the importance of creating safe spaces and making time to have these essential conversations. A specific legacy project creates opportunities for the individual and family* to do just that - to hold on, while letting go. We meet together to explore the impact of the illness, to talk about goals and plans, to acknowledge their grief and honour connections. This project can be completed with families large or small, and include children of all ages. That Project? While the results have been profound, the activity is, quite simply, creating a “Hug”.
The physical embrace of a Hug is comforting for anyone in a time of need. In this instance, it is a creative legacy project that can be completed by anyone, anywhere at any time and is then exchanged as a lasting memento. The Hug can be taken to any significant place or event: to school, a little-league playoff game, during an admission to hospital or hospice, or even once someone has died, these hugs can be buried or cremated and remain with a loved one forever.
Although tantamount to making a scarf, it is more importantly symbolic of the outstretched arms of a loved one, it becomes a personalized “Hug”. The components are basic… a flat sheet, markers or fabric paint, scissors and willing participants. After laying a sheet on the ground, one person lays on top of the sheet while another traces around their outstretched arms and hands. After sitting up, lines are drawn connecting each arm and then taking scissors, cut along the outline. Each Hug is then adorned with messages and images of the shared connection and becomes a tangible expression of their love.
I have completed this activity with anyone wanting to participate, whether ambulatory or bed-bound. For those who are bed-bound, after carefully sliding a sheet behind their shoulders, the family tenderly helps to hold and trace their outstretched arms and hands. Throughout this activity, the individual and family share stories and a profound connection, with each gentle movement and precious memory cultivating an incredibly intimate experience.
Language, distance or time do not serve as barriers. I have completed this activity when families speak a language different from my own. Despite communicating through an Interpreter, the conversation remains seamless throughout as the family creates a beautiful and moving tribute while supporting each other in their shared love and grief. This supportive intervention has also bridged great distances, even though families were thousands of miles apart, they completed and sent their personalized hugs via courier to be at the bedside of their dying loved one. I have also completed this project with children following the death of a parent (many of whom had not been informed about the disease or prognosis in advance). Although a parent - or any loved one might die before the family has an opportunity to have these conversations, it is so important to facilitate therapeutic activities to collectively express their grief while honouring the connection with their loved one.
While this “Hug” is essentially an expressive arts project, it creates and holds significant therapeutic value for all involved. It is a collaborative experience for the family to honour connections while preserving a legacy. Though each experience is unique, what remains universal are the shared laughs, tears and a multitude of stories - whether with a partner, children, grandchildren, siblings, parents, cousins, friends (or all of the above), they create reminders of shared experiences, connections and precious memories.
I believe as Health Care Professionals, we can provide invaluable opportunities for families to connect, and collectively process experiences from time of diagnosis through to end-of-life and into bereavement. I feel extraordinarily privileged that families allow me into their lives - however brief, I hold that time as sacred and do all I can to foster these connections while honouring the legacy of those living and dying.
(family* is defined by the individual - be it partner, children, parents, siblings, neighbour, friend, etc.)
Storytelling in Grief: Honouring Connections while Celebrating Legacies #hpm
“I don’t know how to tell my family about the diagnosis…” “I haven’t told my kids that I’m dying…”
Families often reeling following the diagnosis of Cancer or other life-limiting diseases, struggle with how, and when, to have those essential conversations. I am a Social Worker and for the past 17 years have had the privilege of caring for people facing a life-limiting illness. It is an intimate and profound experience - sitting alongside people as they face end-of-life. They share their hopes and fears - about living and dying - and about caring for and leaving behind those they love. Trying to protect their families but also wanting to prepare them. Whether they speak lovingly about a partner, or children, or siblings, parents or best friends… grieving these losses begins at time of diagnosis.
While treating and managing the disease is important - equally important is caring for the person diagnosed with the disease. What is truly important to them? Who is important to them? How do we provide support in a manner that is congruent with their values and wishes? How do we normalize grief following a diagnosis, and in turn, sit alongside them creating safe spaces - and time - to share their grief should they so choose? As clinicians, we can facilitate supportive interventions at any stage of illness and ideally engage the entire family. Sadly, many families - and specifically many children and youth remain uninformed following the diagnosis of a life-limiting illness, largely resulting from parents need to “protect” and their fear of not knowing what to say. This phenomenon is not rare as it also extends to healthcare professionals, with many reporting fear and uncertainty as to how to best support grieving families and children. This is true whether a child has been diagnosed with a life-limiting illness, or the parent of a child has been diagnosed. Understandably, if the psychosocial needs of families, specifically children and youth remains unaddressed, it only serves to create additional distress for parents and caregivers.
As a Palliative Social Worker I recognize the importance of creating safe spaces and time to have these conversations - to support families in telling their stories, celebrating their connections, and should they so choose, to openly and collectively share their grief. A specific legacy project created opportunities for families to do just that - to hold on, while letting go. I have completed this project with many families facing a life-limiting disease - following diagnosis, throughout the illness, at end-of-life and following the death of a loved one. This can be completed with children of all ages and regardless of the make up of the family - large or small, we meet together and explore their understanding of the diagnosis, the impact of the illness while also celebrating and honouring connections. That Project? While the results have been profound, the activity is, quite simply, creating a “Hug”.
To be clear, this is not a professional boundary violation, but in fact, a creative legacy project that can be done by anyone, anywhere, at any time. In obtaining consent from parents and caregivers, I explain that this is an opportunity for the family to collectively talk about the illness, share stories and experiences, communicate concerns, dispel fears, foster support and enact plans. I introduce this activity as a symbol of their unending love – and the Hug can be taken anywhere - to chemo daycare, during an admission to hospital or hospice, or even once someone has died – this “hug” is also something that can be buried or cremated and remain with a loved one forever…
I assure you this experience is more than a creative activity - it is an intimate and collaborative experience for the family to create a lasting memory. While each experience is unique and the degree to which some “patients” may be able participate varies, in each situation, the family gently accommodates their loved one. What remains universal are the shared laughs, tears and a multitude of stories - reminders of shared experiences and memories of their lives together.
But perhaps I should explain… I feel it is important to outline the essential elements required for this intervention… Specifically, informed consent from the family, clean bed sheets, colourful markers, scissors and glitter. It is simply a matter of laying a sheet on the ground, then a family member lays down on the sheet while another family member traces their outstretched arms and outstretched fingers. After sitting up, lines are drawn to connect the tracings of each arm and then cut along the lines. Although tantamount to making a scarf – it is, more importantly the outstretched arms of their loved one, it is a personalized “Hug”. The child, or partner, sibling, parent or friend then adorns their hug with messages and images and reminders of the shared connection with their loved one - in essence, the “Hug” becomes a tangible expression of their love.
While I involved partners, children, siblings, cousins and friends in this activity long ago I wondered, what if their loved one (or the “patient”, to be clear) also wanted to reciprocate? I began asking patients about this and the suggestion of leaving this touching legacy was always met with resounding approval. While this always requires patient consent and discussion throughout, I have completed this activity with people who were ambulatory as well as people who were bed-bound. While collectively engaging the individual and family, for those who are bed-bound, we carefully slide a folded sheet behind the back of their loved-one. Throughout the activity, the family shares stories and memories, while tenderly helping to hold and trace the outstretched arms and fingers on each hand - every action and movement becomes an incredibly intimate experience. In the case of pathological fracture, we have used the singular tracing of one arm to make a mirror image - completing the hug. Taking that singular hug and laying sheets over top, additional copies are then traced for each family member. This not only engages entire families at the bedside, but also creates a lasting legacy for the surviving family. We often discuss sewing material from favourite blankets, shirts or sweaters on the reverse to preserve a tangible and personal connection.
I have completed this activity when families speak a language different from my own. Despite only being able to communicate through an Interpreter, the conversation remains seamless throughout as we create a beautiful and moving tribute for their family while they collectively support each other in their shared love and grief. While many young couples anticipate milestones like a wedding or the birth of a child, I have also facilitated this project at the bedside of the dying parent together with their young adult children, creating a space to share their hopes and stories while honouring their legacy. This supportive intervention has also bridged great distances, when families were thousands of miles apart. After completing the activity with the patient and family at the bedside, I encourage them to share the idea with extended family and friends across the country and in one specific case, family members of all ages from across the country made Hugs and sent them by courier to the bedside of their dying loved one. Their many colourful “Hugs” surrounded her when she died, each and every one told a story and was on display around her room as a meaningful and tangible connection. Much to the comfort of the family, each and every “Hug” was later buried with her. I have also completed this project with children following the death of a parent, it is especially important for those who were not informed about the illness or were unaware that death was expected. It is so essential to create a space for children to grieve alongside their families to share their thoughts, shed tears, and express the range of their feelings, including grief. We talk about what it feels like to receive hug from someone you love and the opportunity to create a lasting memento to leave with their parent as an expression of their unending connection. Although a parent - or any loved one might die before families and friends have an opportunity to say goodbye, we can still create opportunities for families to collectively share their love and express their sorrow while honouring the legacy of their loved one.
I believe as Health Care Professionals, we have an obligation to provide empathic person and family-centred care. From time of diagnosis we have an opportunity to facilitate honest communication, and in turn, promote adaptive coping strategies for those facing a life-limiting illness. In doing so, we can provide invaluable opportunities for families to connect, and collectively process experiences from time of diagnosis through to end-of-life, and into bereavement. I feel extraordinarily privileged that families allow me into their lives - to share their stories, their love and their grief. However brief our time may be together, I hold that time as sacred and do all I can to create a safe-space to foster these connections while honouring the legacy of those living and dying.
#Palliative Care is not about #dying, but about quality of #living @JMyersPallCare #hpm
There are a multitude of misconceptions surrounding Palliative Care - what it is and what it isn't. Sadly, many are not open to the prospect of Palliative Care because it presented as a departure from "active care" or moreover they believe that Palliative Care is only provided at end of life. It is in fact so much more than that... I truly appreciate this article demystifying the scope and breadth of Palliative Care written by Dr. Jeff Myers, a Palliative Physician, empathic clinician, extraordinary advocate and educator...
"At a time when assisted dying dominates discussion about end-of-life care, I think it’s important to address public fears around palliative care so that people can use the information to improve their quality of life.
Palliative care is not what happens when all treatments have failed. It does not mean “giving up” or “stopping the fight.” If you are fighting cancer or Lou Gehrig’s disease, palliative care means a team of people — such as doctors, nurses, social workers and others — will help make sure you have what you need to continue fighting.
As a palliative care physician, I am deeply committed to improving end-of-life experiences for people and their families. My focus is not on the disease itself but on the impact it can have, like relieving the severity of symptoms with the overall goal of improving quality of life.
It’s my job to know what matters to you and to make sure you’re not spending time and energy on bothersome symptoms that needlessly wear you down. Pain is a good example: terrible pain from cancer can be exhausting, consume a ton of energy and is worse for the body than any medications aiming to manage the pain. There is no need for a person fighting cancer to also try fighting pain.
There is now very clear evidence that people who receive specialized palliative care actually live longer than those who do not. This is why it’s so important to understand that palliative care is not about giving up — far from it. It’s about living the very best you can for as long as you do."
Surviving #Cancer Without the Positive Thinking. Losing Yourself, Seeing the Beauty and the Love @embeedub
"My husband and I were always transparent with the kids. They saw me cry; they saw me get scared. We used words like died rather than passed away. Now I see the kids as these amazing, compassionate, clear-eyed people who know how to comfort others and who have made space in their life for death. That is so unusual in our culture. I want my kids to have a relationship with the fluidity of life—with the fact that sometimes people get sick and sometimes bad things happen, and to know that within that there is also grace, there’s also beauty, there’s also comfort. Because if you go down into the depths, there is treasure there. Cancer still sucks, but there’s also profound connection. It’s the privilege of allowing yourself to participate in the full experience of humanity, which includes grief and sickness and death. If you don’t look at [those things], you’re not living...
There’s this assumption that because you got better, you did it courageously. But that’s not my story. I didn’t “warrior” my way into getting better. It was not my achievement; it was science’s. Whenever I hear someone say “I beat cancer,” it just feels so disrespectful to others, such as my friend Debbie. It divides us into winners and losers. I know it’s not deliberate. We want to make meaning. We want to make sense of it. But you see how random [survival] is. I have known people who were healthier than me and younger than me who tried, I think, harder than I did to fight their cancer but who didn’t live…
The story is about losing something—yourself, people you loved, what you thought you knew about the world—yet still being whole. Butterflies are all about transformation. I try to see the beauty in all the damage. I try to see the beauty in all the ruin. And I definitely see the love."
I can’t save my daughter from a terminal illness. But we can help save other children from the same fate.
"There is no way to escape losing a sense of who you once were. And after a year (or two), you wake up from this transformation and realize that you were not actually dying; you just felt like you were. And then you must make a choice. One option: You can give into the horror of it all and retire to bed. No one would blame you; it is a tempting alternative that lurks at the back of my brain from time to time even now. The other option is that you take the pain and harness it to do things you could not imagine ever possessing the strength to accomplish. Being around children like my daughter will teach you the very meaning of life."
Talking About #Death Won’t Kill You. @Kathykm @TEDTalks #Death #Education #hpm
"An unconventional death educator with an equal parts wry and wise delivery style, Dr. Kathy Kortes-Miller is committed to showing her audience that talking about death and dying won’t kill you. Using stories and research, Kathy extends an invitation to view death as not a taboo subject - but rather a shared life experience. Audience members walk away with shifted perspectives and a deep understanding that talking about death, without knowing or needing all the “answers”, actually brings us closer to our loved ones than we ever imagined possible."
When the #Patient Won’t Ever Get Better @danielalamasmd #hpm #ACP
“In the early moments of critical illness, the choices seem relatively simple, the stakes high – you live or you die. But the chronically critically ill inhabit a kind of in-between purgatory state, all uncertainty and lingering. How do we explain this to families just as they breathe a sigh of relief that their loved one hasn’t died? Should we use the words “chronic critical illness”? Would it change any decisions if we were to do so? Here, I find that I am often at a loss.
I was quiet on the other end of the phone line that night. Was my patient stable? For the moment, she was. But with each event like this one, and there would be more, my patient would move further from the hope of ever reclaiming that life she had had in the fall: living in her own home, watching movies, cooking. I felt that I could see the weeks and months spooling out, a moment of calm, a new emergency. But this wasn’t the time to tell her daughter, not on the phone, not tonight.
And so I told her the truth – one truth, at least. Her mother was critically ill, but stable for the night”.
Lessons for the #Living: On #Dying and Dinner Parties @elderlyprograms #hpm
The Sky Isn’t Falling @Speed4Sarah in @brainchildmag on her #diagnosis of #ALS.
“I was spinning, untethered from the person I felt I had once been. A marathon runner, a devoted mom and wife, an independent woman who had never particularly liked asking for help. I was consumed by my sadness and confusion, by my anxieties about what was to come.
And then I discovered other people who were like me. Young moms and dads, people in their 20s who never had a chance to start a family, all of them living with ALS. I found them by writing about my experience, by joining a group on Facebook, and by becoming heavily involved with several nonprofit organizations that raise money for ALS research. My people, it turned out, were not the ones in the senior home who had lived long lives and had much to show for it. My people were the ones who were fighting for their lives, fighting for more time with their children, fighting a disease that we’d been told would certainly kill us–and soon”.
#Canadian Virtual #Hospice. Information and #Support on #Palliative and #End-of-Life #Care, #Loss and #Grief. @VirtualHospice
#Memories of a #Caregiver - Honoring Voices: Walking Alongside The #Caregiver. #hpm
Are #Families Ready For The #Death And #Dying #Conversation? #ACP #InformedChoice
"The Institute of Medicine (IOM) believes the time is right for a national dialogue to normalize the emotions on death and dying. They think that the social trends point toward a growing willingness to share stories about the end-of-life care and that it will help drive more family discussions. In the IOM consensus report, Dying in America, experts found that accessibility of medical and social services could improve a patient’s life at the end. But if people don’t discuss which medical care or social services they want or not, how will their wishes be known and carried out?"
How to Tell Someone You’re #Terminally #Ill. #hpm
"Though everyone eventually dies, few know how to talk about the end of life. ‘‘People don’t know what to say,’’ Wanda says. ‘‘They’re afraid.’’ Be prepared for strange and stilted reactions. Some want to believe in a fix and will give you unsolicited health tips. (‘‘Don’t eat sugar.’’ ‘‘Avoid gluten.’’) You can ignore their suggestions but acknowledge the heart underlying them. People may offer to pray for you. ‘‘Prayers are good, but maybe what I need is someone to listen,’’ Wanda says. For that type of engaged listening, you may need to seek out a professional, like a trained social worker or a psychiatrist. Sometimes people who know about your condition — those you tell will tell others — will pretend your situation does not exist. Or weirder still, they will temporarily forget".