Thank you to Wellspring Niagara for the invitation to present “Demystifying Palliative Care: Exploring a Wrap-Around Approach to Quality of Life”.
It is important to acknowledge the barriers exist - to education, services, funding & resources.
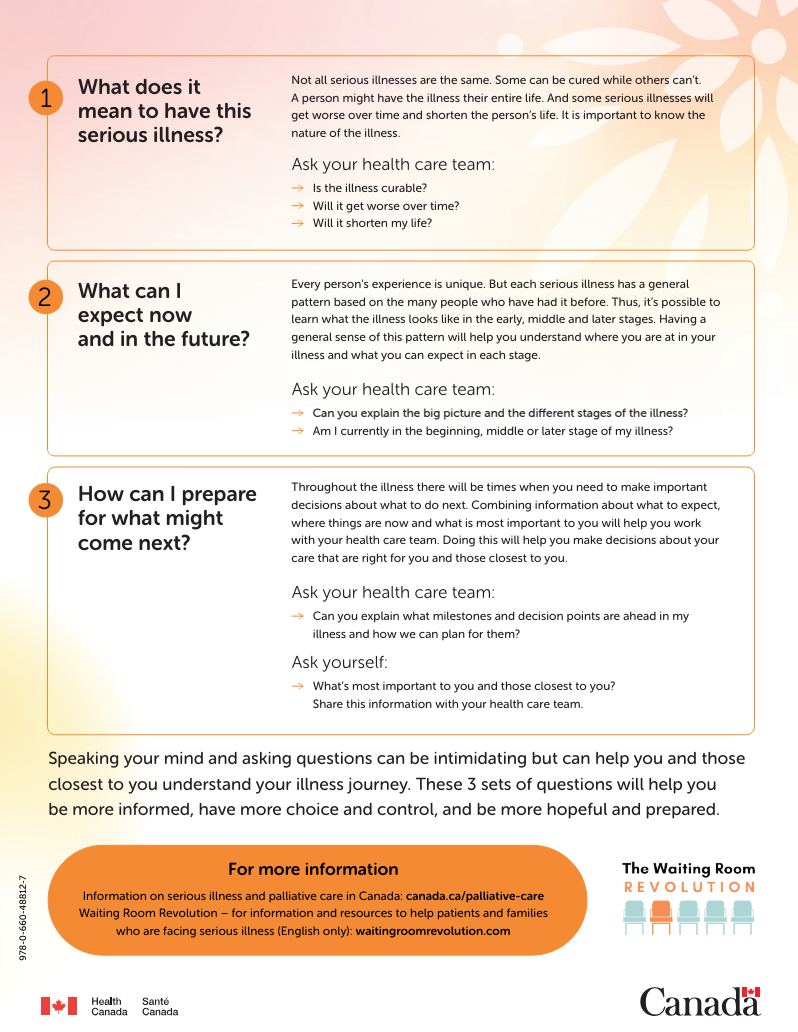
Did you know that Palliative Care is:
Appropriate for any person & or family living with, or at risk of developing, a complex illness due to any diagnosis, with any prognosis, regardless of age, & at any time they have unmet expectations & or needs, and are prepared to accept care
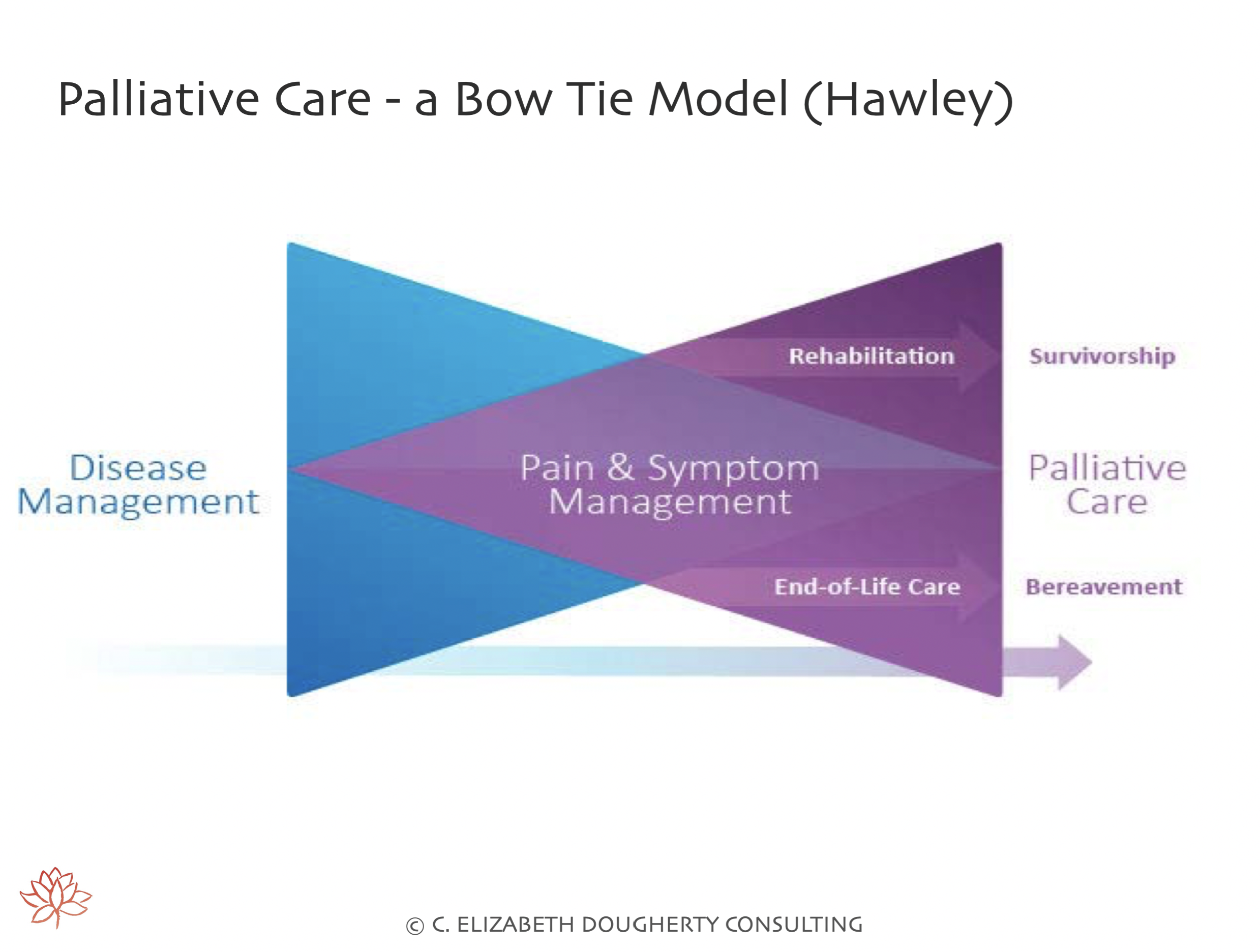
May complement & enhance disease-modifying therapy, OR it may become the total focus of care
Most effectively delivered by an interprofessional team who are both knowledgeable & skilled in all aspects of the caring process related to their discipline
Treats all active issues & prevents new issues from occurring
Addresses physical, psychological, social, spiritual and practical issues, & their associated expectations, needs, hopes & fears
Prepares for & addresses self-determined life closure & the dying process;
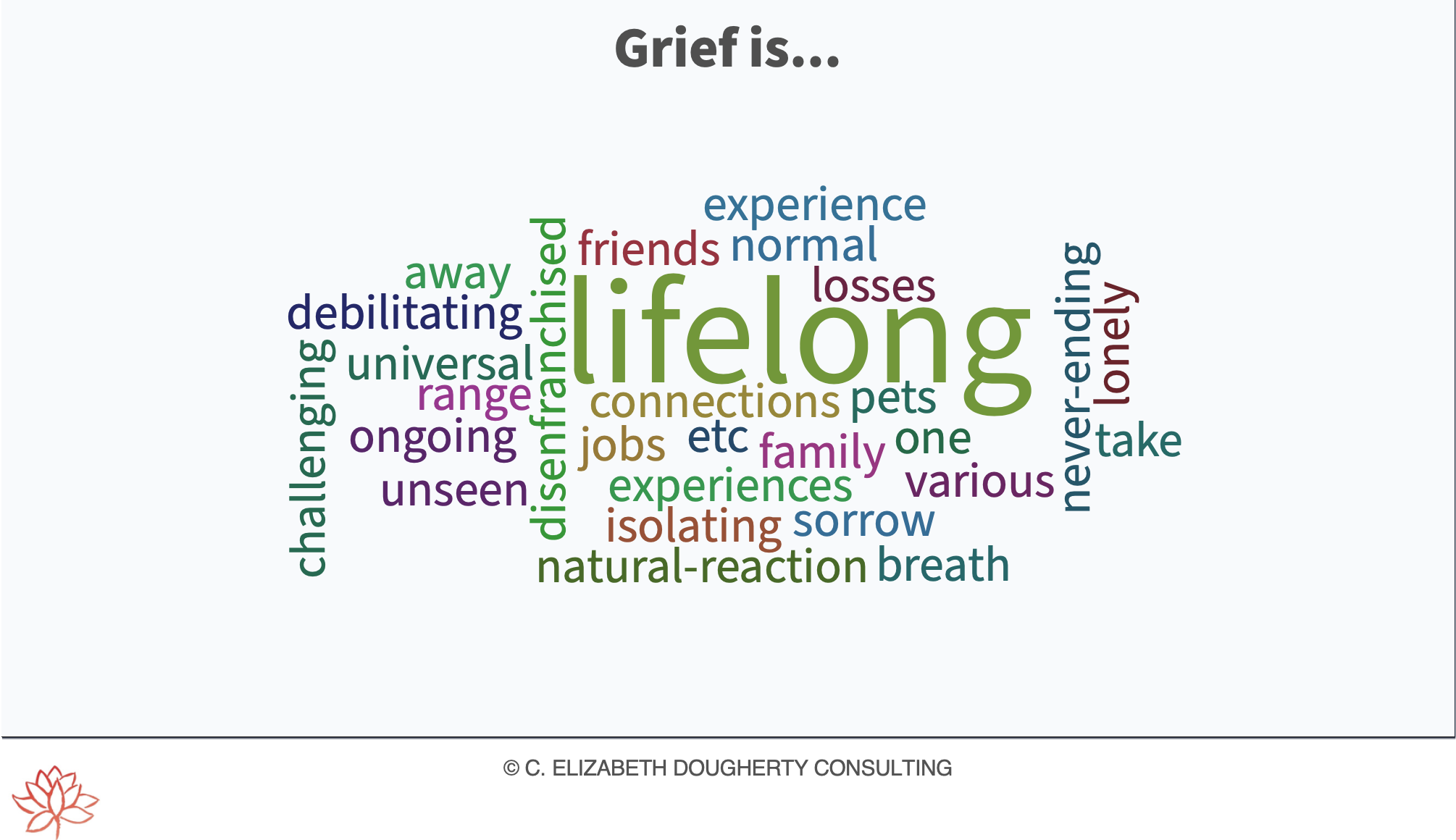
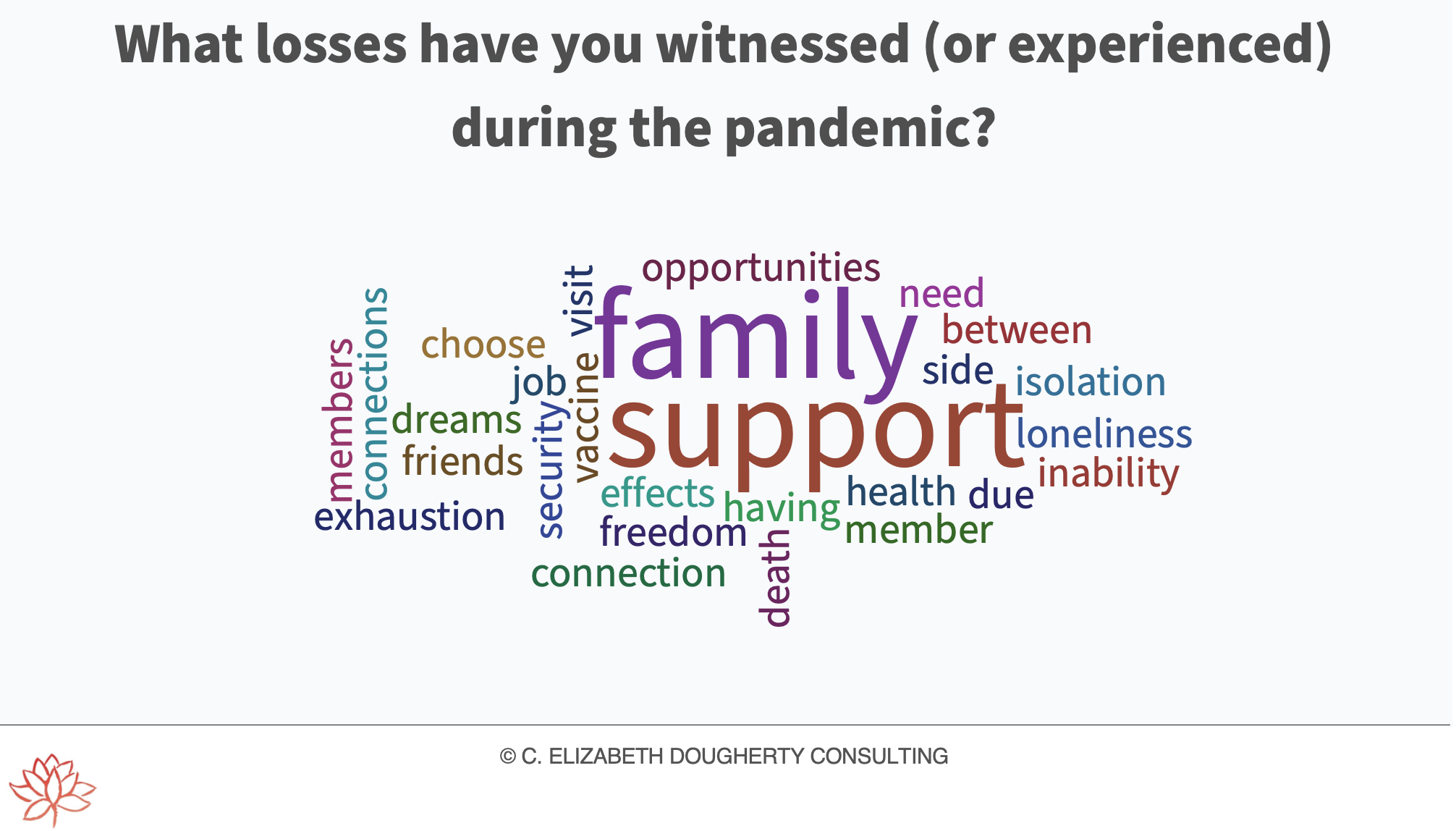
Assists in coping with loss & grief throughout the illness & into bereavement
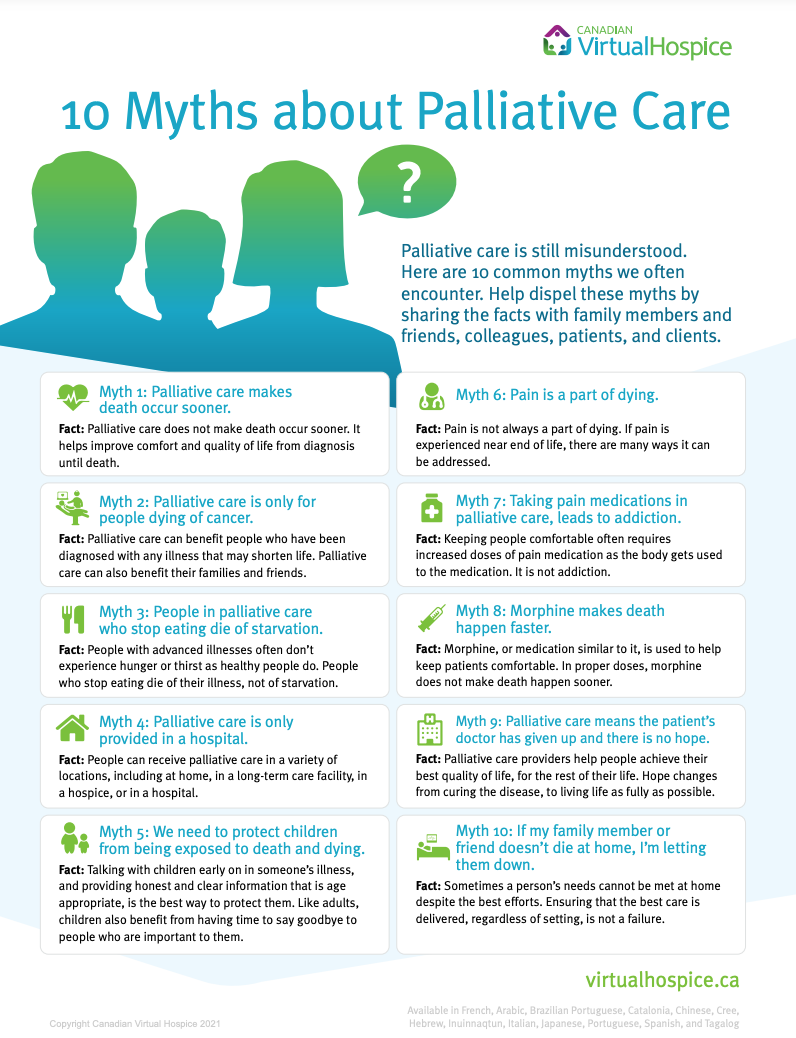
Yet SO many barriers exist, including:
Few Canadians (15%) have EARLY access to Palliative Care
Palliative Care provided during admission to hospital was unplanned or through an emergency department 80% of the time
62% of Canadians who received Palliative Care did so in an acute care hospital in their LAST month of life
Palliative Care is a patchwork of uncoordinated services
Palliative & end-of-life care remain underfunded - receiving only ~1% of the overall investment in cancer research
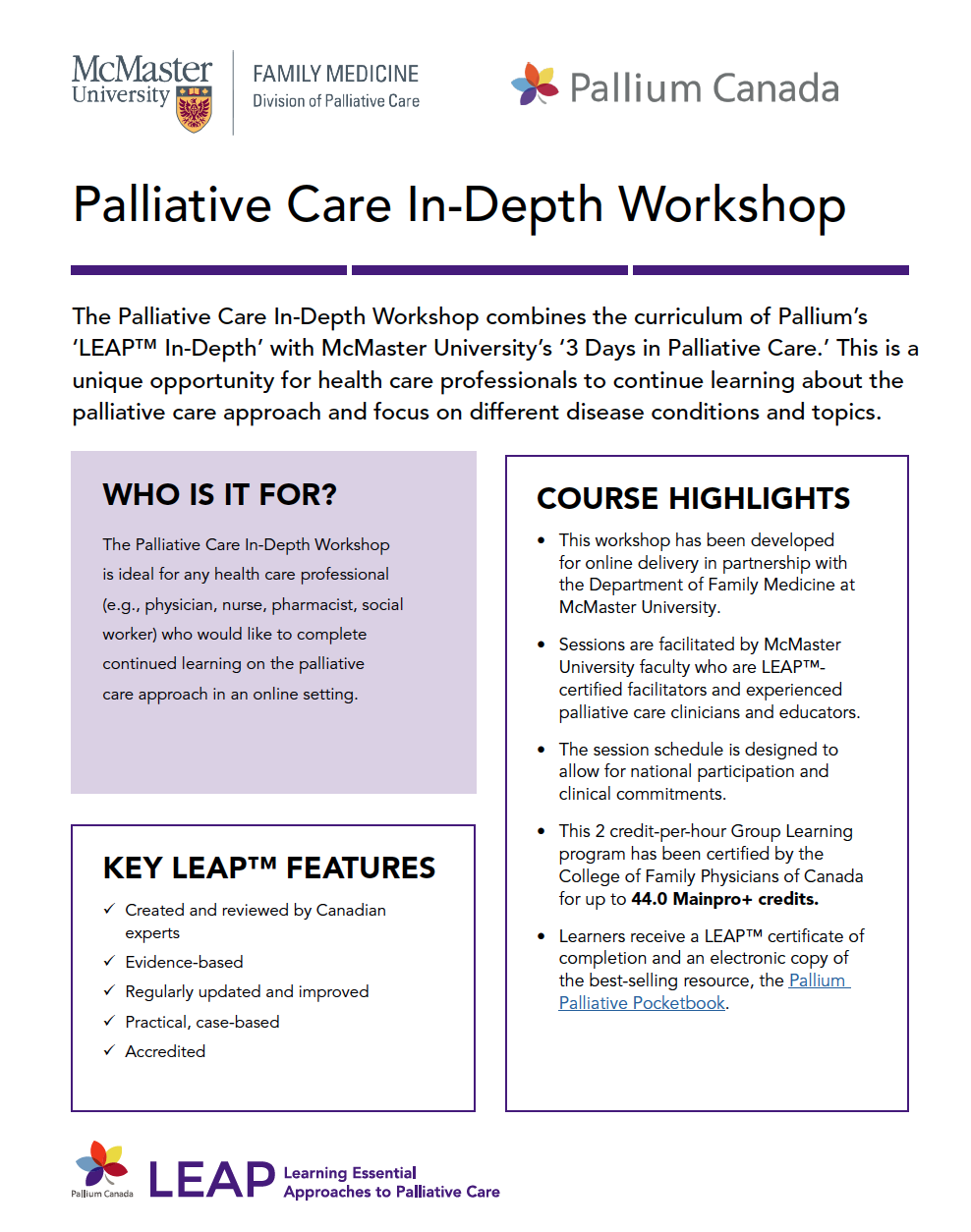
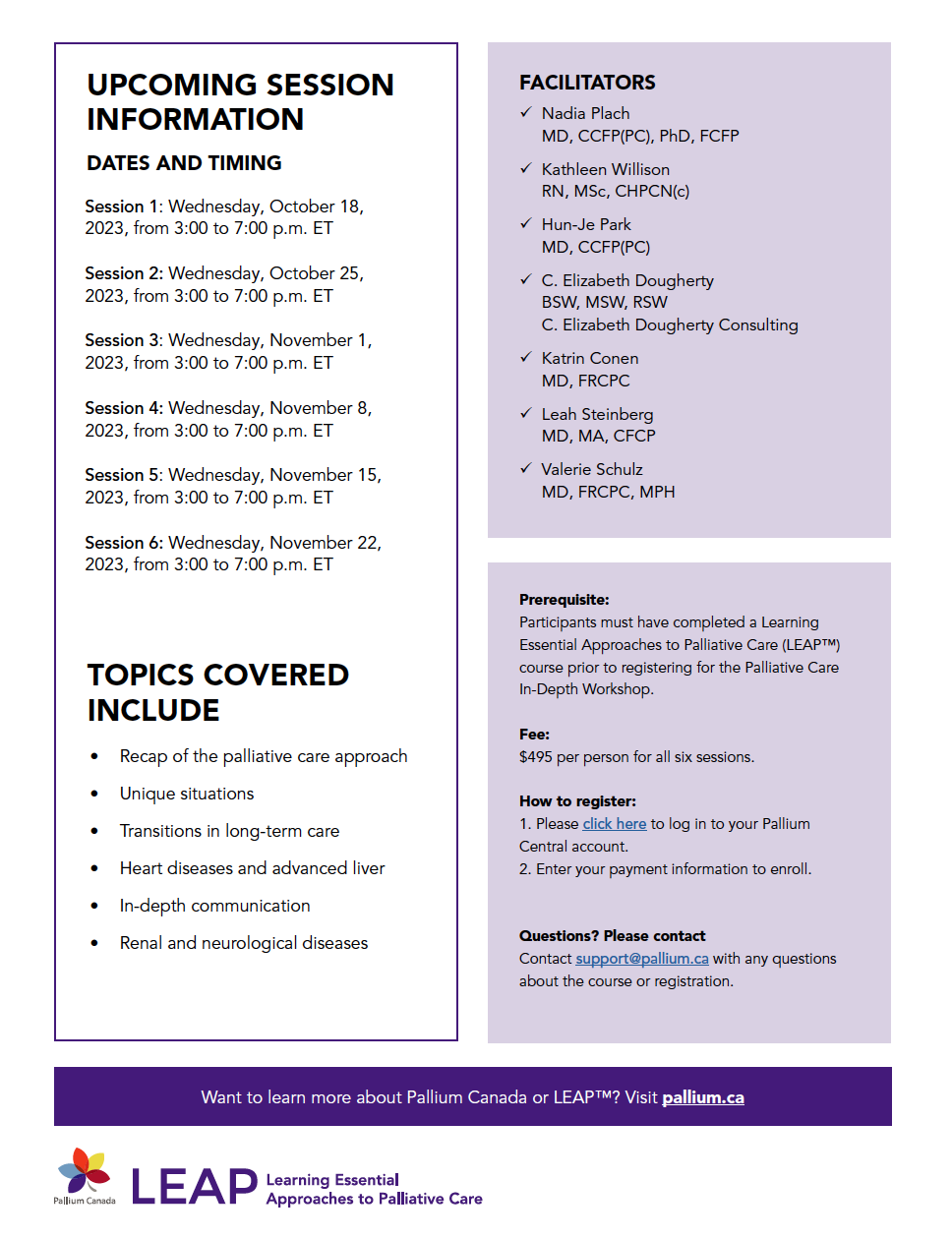
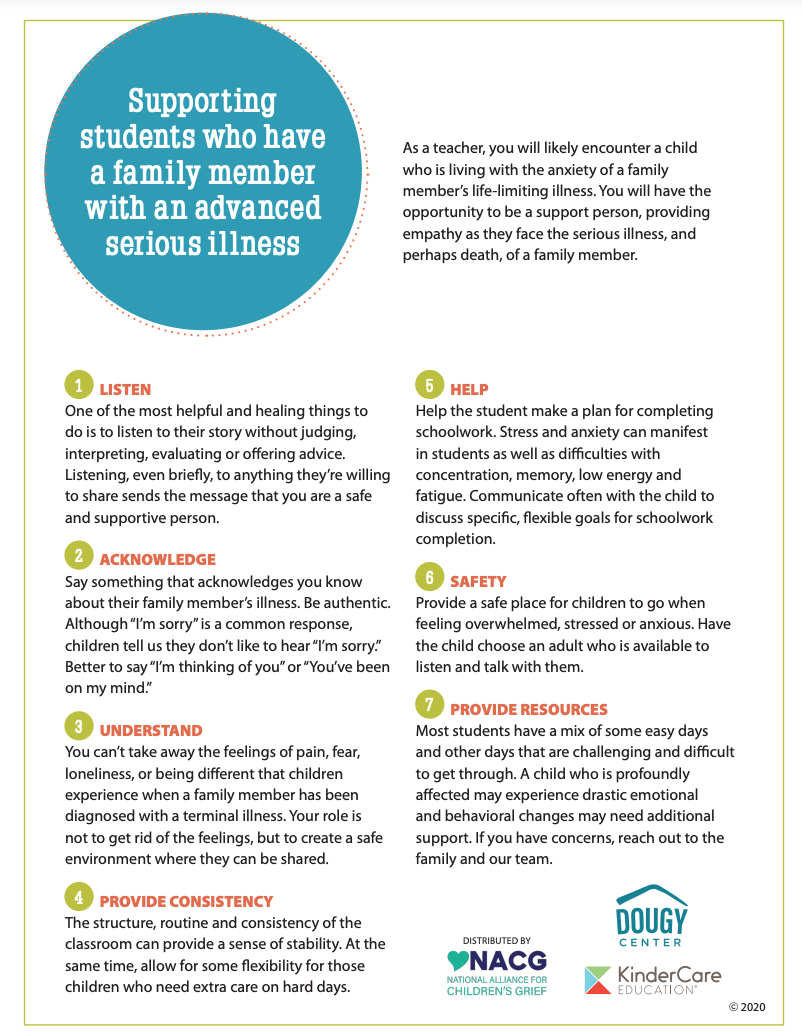
Mandatory education should be required for ALL healthcare providers due to the team-based nature of high-quality palliative care, including culturally safe palliative care, grief & bereavement supports
Structurally vulnerable & marginalized communities including: Unhoused people, Indigenous communities, non-English speaking patients, young patients & 2SLGBTQ+ individuals & families face additional barriers to care resulting in inequitable access.
It is essential that we address barriers and stigma surrounding Palliative Care as this impacts access to care - for anyone facing a complex illness (curative or life-limiting).