"Oncologists, cardiologists, and other specialists can often predict a patient’s rate of decline based on a specific disease, Obermeyer said. But patients, particularly those who are elderly, often suffer from more than one serious illness that make it more difficult to predict when they’re near death. So a pulmonologist might treat someone’s pneumonia, for instance, without recognizing it signals a broader decline".
"A parting lesson from my parents". ~Andrew Dreyfus
"As I have become more involved with this work, I have wondered whether the CEO of a large health plan is the right person to talk about end-of-life care. But I only have to remember how important this issue was to my brother and my parents to realize that — in this case at least — my personal experience should inform my professional actions. Everyone, regardless of economic, cultural, racial, or geographic differences, must have their choices and values heard and respected. Everyone deserves the chance to live the best life possible, to the very end".
Dignity, Respect and Choice: Advance Care Planning for End of Life for People with Mental Illness.
"Dignity, Respect and Choice: Advance Care Planning for End of Life for People with Mental Illness is a two part resource that will help support people with mental illness, their families and carers, and health professionals with the complex issues which might arise around Advance Care Planning for End of Life".
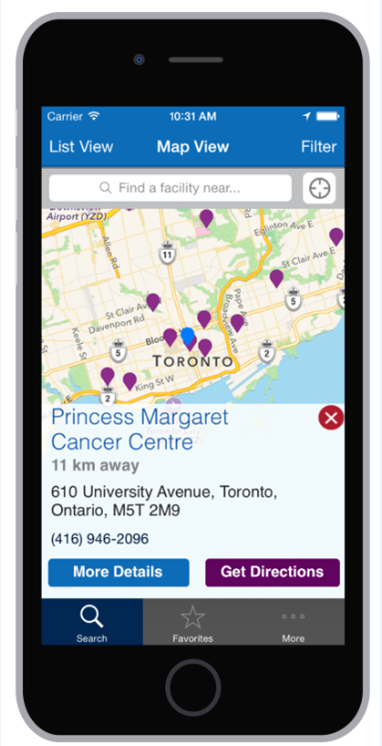
Inpatient Hospice Palliative Care Directory free via iOS and Android.
"Although some people hope to remain at home for the duration of their illness, many people find that admission to an inpatient setting can also be helpful. The inpatient care settings in the directory include palliative care units, residential hospices and dedicated palliative care beds within local hospitals. Inpatient hospice palliative care support includes 24 hour care, specialist pain and symptom management and psychosocial support for patients and families.
The map provides access to a directory which includes more information about inpatient hospice palliative care settings across Ontario. The list of facilities below may not be complete - there may be hospice palliative care settings which are not in the directory.
For contact information and details about the facility, click on a specific location. If you want more information, contact the hospice or palliative care program directly".
Bearing Witness to Suffering. ~ Laura van Dernoot Lipsky
In this talk, Laura offers us a window into the cumulative toll that can occur when we are exposed to the suffering, hardship, crisis or trauma of humans, other living beings, or the planet itself. Held within a larger context of systematic oppression and liberation theory, we'll dive into what gets hard and how to work toward reconciling it both individually and collectively.
The Way Forward: An Integrated Palliative Approach to Care.
Palliative Care Sooner for Patients But Also for Medical Professionals.
"Changing culture is a process. Awareness and understanding of palliative care is often limited, yet the benefits are discernible from better quality of life to care more consistent with patient preferences, to more recent data indicating improved survival. My experience with palliative medicine as a first-year medical student has made me realize how vital palliative care education could be for all medical students".
The Paternalism Preference — Choosing Unshared Decision Making.
"Consent is not merely the granting of permission but an exercise in choosing, and choice requires disclosure of a certain amount of information. How much information is adequate? Rather tautologically, as much as necessary to decide: 'The scope of the physician's communications to the patient must be measured by the patient's need, and that need is whatever information is material to the decision'.”
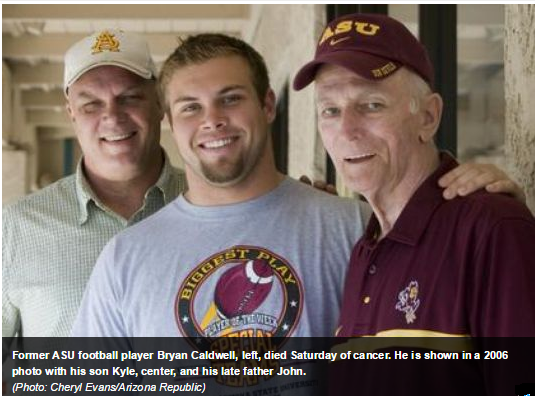
Finishing Strong: Moments of Life Made Possible by Hospice.
"In September 2012, Bryan Caldwell was diagnosed with Hodgkin’s Lymphoma. A former professional football player in the NFL, rancher and surfer, he embodies strength. His wife, Krista, a nurse with Houston Hospice El Campo, even tells the story of how the morning before he was diagnosed, Bryan mowed the yard with a collapsed lung.
Six months into his fight with lymphoma, Bryan learned his cancer was unresponsive to medical treatments. He knew he wanted to spend his remaining time living without pain, at home, surrounded by all he loved. So he chose hospice care.
'Our whole philosophy is not to stay sitting, it’s to stay moving and to keep living each moment that comes along,' says Bryan. 'Hospice provides that golden opportunity for me, every single day. If I have the energy and I feel up to it, I’m getting out there'.”
Trauma Workers Find Solace In A Pause That Honors Life After A Death.
"Jonathan Bartels is a nurse working in emergency care. He says witnessing death over and over again takes a toll on trauma workers — they can become numb or burned out. So the next time we worked on another person who didn't make it, I decided to be bold and stop people from leaving," he says. "I just said, 'Can we stop just for a moment, to recognize this person in the bed? You know, this person before they came in here was alive — they were interacting with family, they were loved by others, they had a life.' "
The team did it. Standing together silently, they stopped — just for a minute.
"When it was done, I said, 'Thank you all, and thank you for the efforts that we did to try and save them.' People walked out of the room, and they thanked me," Bartels says.
What's come to be called The Pause is now being taught as part of the curriculum at the university's nursing school. Emergency medical technician Jack Berner says it helps him handle the toughest cases. ‘It makes it so we can actually view the person as a person, rather than as a patient that we see on an everyday basis,’ he says. ‘You can relate more to the case, [knowing] it's somebody's father or their mother, their sister or their uncle, rather than somebody you just see for five minutes’."