"There are apps for nearly everything -- ordering food, catching rides and finding dates, to name just a few of the common tasks people accomplish via a swipe of a screen. Now, a Boston-based company wants to make thinking about and planning for death just as simple.
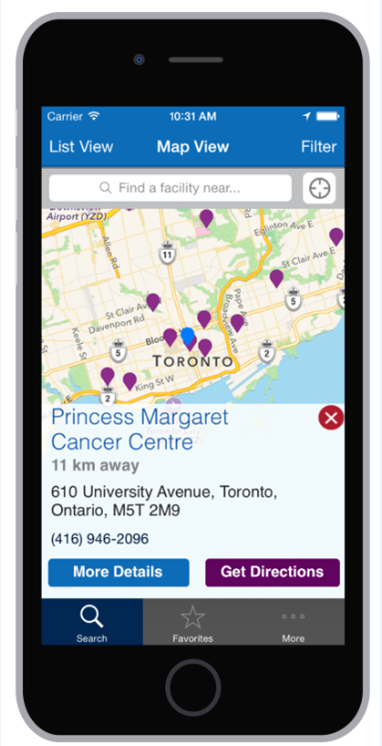
Cake, as in “a piece of cake,” is a website and soon-to-launch app that asks people a series of yes-or-no questions about the end of their lives in order to help them think about certain issues, plans and needs. The topics include funeral preferences and financial planning, as well as whether there are places people want to see before dying and how satisfied they would be with their relationships if they died tomorrow.
'One of the biggest problems right now is that even if you want to have these conversations, most of us have no idea where to start. It's daunting and overwhelming,' Chen said.
'Even though we know ourselves, we may not truly understand our own values around end of life because most of us haven't spent much time thinking about it. We developed the app as a way to ease people into thinking about the end of life'.
The app is targeted toward users who want to talk about dying to their loved ones, as well as those who want to share their end-of life-wishes with their doctors and caretakers.
'We interviewed dozens of health care professionals and routinely heard doctors say that bringing up advance care planning ‘is the hardest part of my job.’ Even doctors who are trained in how to have these conversations find it challenging to bring up,' Chen said. 'Additionally, there's often not a lot of time at the doctor's office. It makes sense to provide a synchronous tools that empower people to think about things on their own and with their families while they're in the waiting room, or at home'.”