"The essential guide for every patient and family.
When you are diagnosed with a life-changing illness, it can be overwhelming. While your diagnosis cannot be changed, the way you experience your illness can.
In Hope for the Best, Plan for the Rest, we draw on our decades spent researching and caring for thousands of seriously ill patients to reveal the seven keys for a better illness experience. With real-life stories, tips, and exercises to improve your journey right from diagnosis, we want to empower you with practical tools to navigate the healthcare system with knowledge, confidence, and clarity.
You can find hope in the face of uncertainty. You can live well, be fully informed, and be activated - and feel more like a person and less like a patient. But most of all, you can be hopeful and prepared at every step along the way."
Source: Waiting Room Revolution
April 16th is Advance Care Planning Day in Canada
Planning for future healthcare needs is important.
Who would you trust to make healthcare decisions?
Do you know what would happen if you couldn’t communicate for yourself?
Who would you trust to make those healthcare decisions on your behalf?
Think about:
Who you would trust with making important decisions for you.
What matters most in your life and how that might help guide healthcare decisions you would want.
Consider:
Do you know what would happen if you couldn’t decide for yourself?
Who do you trust to make healthcare decisions that respect your wishes?
Would that person (or people) be able to make important decisions about your health in an emergency?
Have you spoken to anyone about what matters most in your life?
What gives you strength in difficult times?
Are spiritual, cultural or religious beliefs, practices, or ceremonies are important to you?
The best time to think about this is NOW (in advance of a medical crisis), while you can make decisions and communicate for yourself. You have the power to choose who that person is. They can be a family member, a friend, or anyone in your life that you trust to make the kinds of healthcare decisions you would want.
Ask yourself: If not you, who?
Source: Advance Care Planning Canada
It is never too early, but it can be too late!
To learn more about Advance Care Planning in 5 Steps, visit Advance Care Planning Canada to access helpful free toolkits and guides to help you along the way.
Exploring the Role of Social Work in Palliative Care
So grateful to speak with my friends and colleagues Drs. Hsien Seow and Sammy Winemaker on their podcast The Waiting Room Revolution.
We explored the role of Social Work in Palliative Care, the value of proactive and compassionate person and family-centred support following diagnosis of any serious illness, exploring loss and grief through to end-of-life and bereavement, creating space for essential conversations, and the healing power of silence.
Follow their podcast for essential tips and tools to navigate the healthcare system following diagnosis of a serious illness. To listen to our conversation, click here
COVID-19 Response – Free, Online Palliative Care Modules from Pallium Canada
Enhance your knowledge, skills, and practice in providing high-quality palliative care with these free, self-directed modules.
Pallium, in collaboration with the Canadian Medical Association (CMA), is providing access to essential education on palliative care for all health care professionals in response to this unprecedented COVID-19 pandemic. In these difficult times, it is more important than ever that all health care providers are equipped with the essential skills to provide compassionate, palliative care to patients in need.
Available modules
These modules are self-directed and completed at your own pace:
Taking Ownership
Advance Care Planning
Decision-Making
Managing Dyspnea
Palliative Sedation
Last Days and Hours
Additional Information
Pallium and CMA are making these 6 Learning Essential Approaches to Palliative Care (LEAP) modules available online for free to all health care professionals for 3 months (March 30 – June 30, 2020). These modules will help provide health care teams with an introduction to the palliative care approach focused on the important knowledge and skills required during the COVID-19 pandemic response. The modules are currently only available in English.
The Pallium Palliative Pocketbook can be found here. This best-selling book is a practical, one-stop resource with easily accessible information to help non-specialist physicians, nurses, pharmacists, and social workers provide a palliative care approach when needed.
Additional learning opportunities to help you expand your knowledge in palliative care can be found on Our Courses page, including our newly available LEAP Online course.
Have any questions? Email anytime at: info@pallium.ca
Source: Pallium Canada
Death Cafe for healthcare professionals, health science students or healthcare volunteers
Excited to be facilitating another Death Cafe for the Division of Palliative Care, McMaster Faculty of Health Sciences at McMaster University.
If you are a Healthcare Provider, Health Science Student, Hospice Palliative Care Volunteer or Funeral Service Employee, this Death Cafe is specifically for you!
A Death Cafe is a group directed discussion of death with no agenda, objectives or themes. It is a discussion group rather than a grief support or counselling session. The objective is 'to increase awareness of death with a view to helping people make the most of their (finite) lives'. Source: Death Cafe
Please join us at this FREE event at the David Braley Health Sciences Centre on Wednesday, July 24th from 6-8pm as part of our Public Health Palliative Care Elective.
Please help spread the word. While the event is free, registration is required via Eventbrite: https://www.eventbrite.ca/e/death-cafe-tickets-62361840945?fbclid=IwAR2aqlWTC8CcDPU4TKspXU3hZC65Om4ZxZZikvgh9ztqz3TEUe9GJcFLJ00
Function in the Midst of Dysfunction: Supporting Families Facing Serious Illness
#BustingTheMyths about Hospice Palliative Care
It’s Hospice Palliative Care Week in Canada.
The campaign (May 5th – 11th) this year focuses on #BustingTheMyths about Hospice Palliative Care
This year, the Canadian Hospice Palliative Care Association (CHPCA) designed a “Busting the Myths” campaign as a response to the need to educate Canadians including caregivers, physicians and all healthcare providers, citizens and political leaders around common myths about hospice palliative care.
The #BustingTheMyths campaign aims to empower Canadians through education by identifying and clarifying misperceptions about Hospice Palliative Care in Canada.
Working together to educate one another is a vital step in the pursuit of excellent Hospice PalliativeCare.
Source: CHPCA Canadian Hospice Palliative Care Association
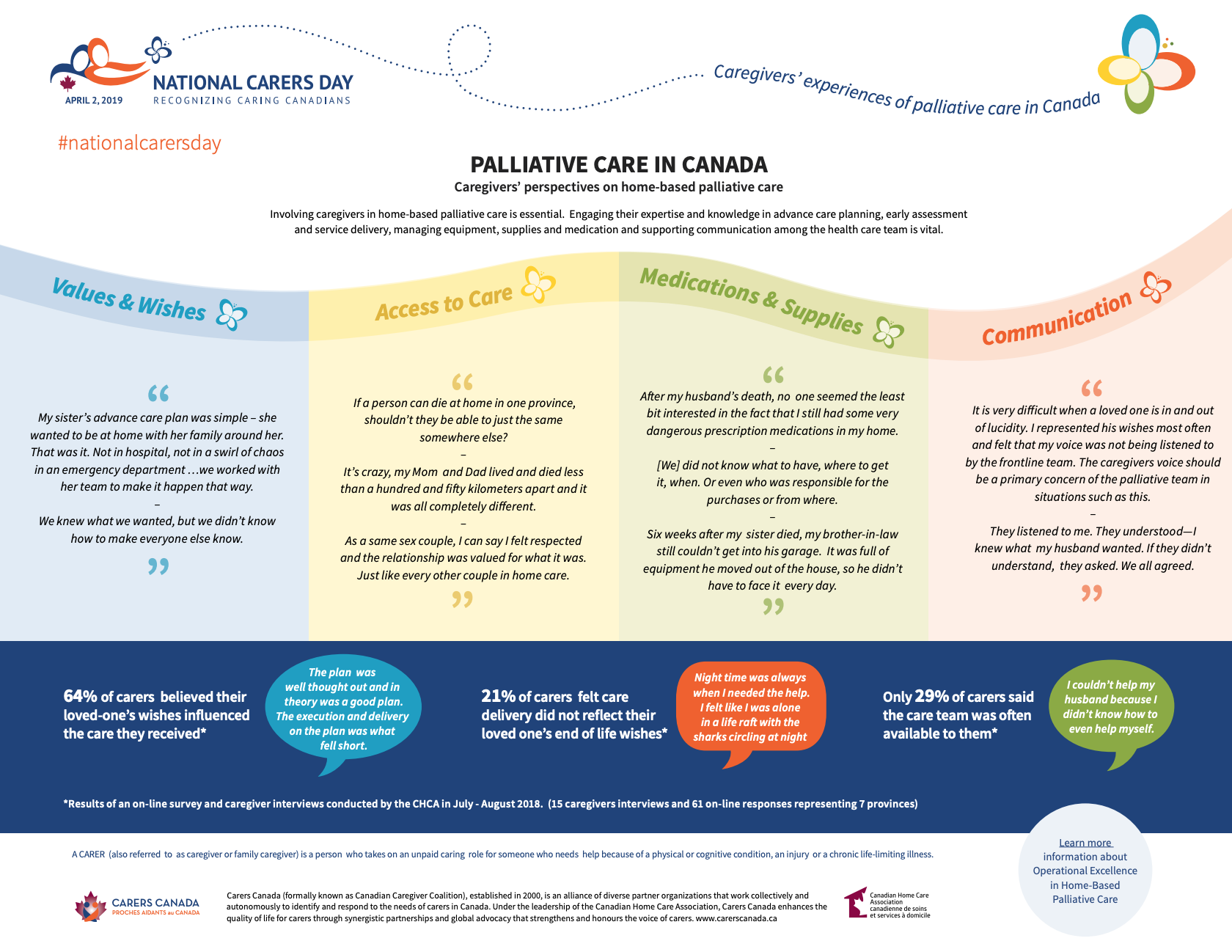
April 2nd is National Carers Day
About National Carers Day
In April 2010, the Parliament of Canada unanimously adopted a motion declaring the first Tuesday in April “The Invisible Work Day.” This day was designated to recognize the importance of the “invisible” unpaid work carried out by parents and caregivers on behalf of their children and aging family members, as well as the volunteer work done in the community. Recognizing that caregivers come from all walks of life and take on many roles, the first Tuesday in April is a special day where we can recognize all caring Canadians.
#NationalCarersDay
End Game Documentary and Discussion
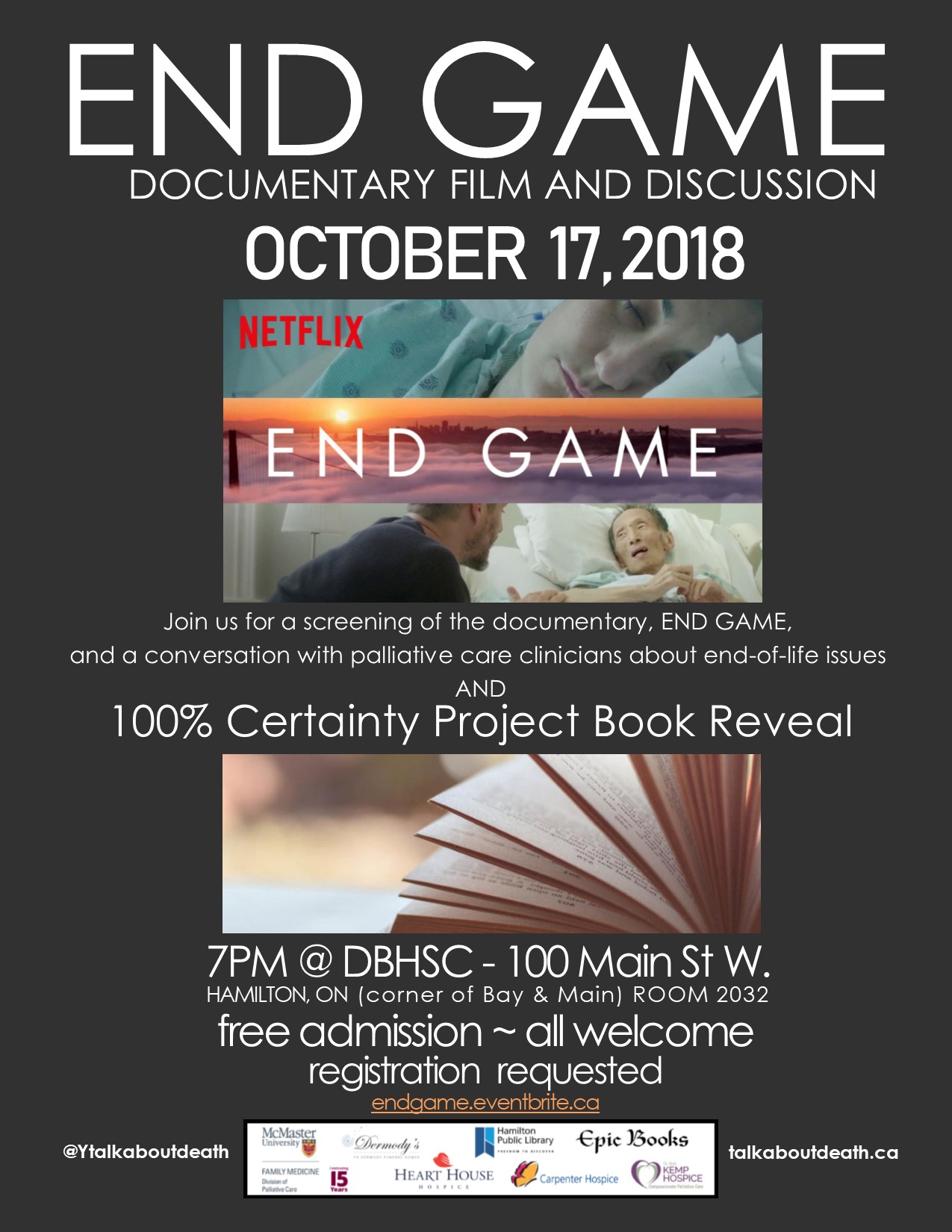
Excited to co-host and participate on the panel for the launch of the 2018-9 season of "The 100% Certainty Project. Death: Something to Talk About". Join us for a screening of the Netflix documentary, "END GAME" followed by a conversation with Palliative Care clinicians.
Our free public event at McMaster University features the brilliant documentary "End Game" from Shoshana Ungerleider, MD highlighting the essential tenets of Hospice Palliative Care. The film showcases the collaboration, compassion and communication as the heart of person and family-centred care at UCSF Medical Center with Steven Pantilat and the extraordinary interprofessional team. The film also highlights the brilliant work of Zen Hospice Project, showcasing Dr. BJ Miller and the extraordinary interprofessional team in Hospice.
Please join us for this engaging event! While the event is free, registration is required via Eventbrite via https://www.eventbrite.ca/e/end-game-documentary-and-discussion-tickets-50535681584
Almost all Canadians would benefit from palliative care. Only one in seven can actually access it at end-of-life
“The key to providing decent palliative care is a little bit of basic planning. Four conditions – cancer, cardiovascular disease, COPD (lung disease) and diabetes – account for 70 per cent of deaths.
Those chronic conditions all have fairly predictable courses of illness in the terminal phase. You don’t get diagnosed with lung cancer or heart failure one day and die the next. It’s a months-long process and providing pain relief (palliation) should be standard, and a priority.
Two in three people receive home care in their last year of life. But only one in seven receive palliative care in the home.
That’s the failure point – and that’s what we need to fix.
There needs to be a commitment – philosophical and financial – to bringing palliative care to patients when they need it and where they want it.
Not everyone can (or should) be cared for at home in their final days. It’s back-breaking, emotionally-draining work for loved ones. Yet many would do so willingly and lovingly.
But they run up against a gross number of barriers, ranging from difficultly getting home visits from physicians (who are poorly remunerated for that work in many provinces), lack of nursing support (because of caps on home care hours), and absurd rules that mean drugs taken at home are not covered by medicare.
All the problems raised by the CIHI report are easily resolved. For example, having paramedics provide palliative care can eliminate transfers to hospitals. Sending doctors and nurses to homes or nursing homes can free up hospital beds – and save money in the process. Not to mention that, at the very least, people deserve a modicum of dignity in their dying days.
The whole point of palliative care is to improve quality of life. We shouldn’t let bureaucratic and structural inadequacies undermine that necessary and noble work.“ by the brilliant André Picard via The Globe and Mail
Professional Competencies with the Michael G. DeGroote School of Medicine at McMaster University
Thrilled to be teaching Professional Competencies with the Michael G. DeGroote School of Medicine at McMaster University.
"In Pre-Clinical studies, Professional Competencies (Pro Comp) runs in parallel to the Medical Foundations. Groups of 8-10 students work with a pair of facilitators, one MD and one a clinician from a different discipline. The groups stay together for the entirety of Pre-Clinical, meeting every Tuesday morning for 3 hours. They explore material covering seven domains: effective communication, medical decision-making, moral reasoning and ethical judgement, population health, professionalism and self-awareness and self-care, interprofessional practice and social, cultural and humanistic dimensions of health." via https://mdprogram.mcmaster.ca/mcmaster-md-program/what-is-compass2/pre-clinical/pro-comp
Patients feel psycho-social impact of chemo more acutely than physical side effects
Highlighting the need for integrated Person and Family-Centred Care...
"The results show that there might be a gap between what doctors think is important or disturbing for patients, and what patients really think. Physical, psychological, social and spiritual support is needed at every stage of the disease"
Source: Patients feel psycho-social impact of chemo more acutely than physical side effects. MedicalXpress
What can Palliative Care Do?
"When you are facing a serious illness, you need relief from symptoms. You need to better understand your condition and choices for care. You need to improve your ability to tolerate medical treatments. And, you and your family need to be able to carry on with everyday life. This is what palliative care can do." #SeriousIllness #PalliativeCare
For more information visit Get Palliative Care
Informed Patient? Don’t Bet On It
"We’ve seen too many patients regret decisions that they made without fully understanding their options, or the possible outcome. We encourage our patients, and our colleagues, to be partners in what are often life-changing decisions about health care."
Read the full article The New York Times
5 ways to improve care at the end of life
"All of us face the difficult prospect of a parent or loved one suffering from an illness that ultimately leads to death. When that time comes, we will want to ease their physical and emotional pain, respect their wishes, and allow them to die with dignity — the same things we will want for ourselves.
The way that Americans die has changed but, unfortunately, our medical system hasn’t kept up. It was designed at a time when death was often sudden or declines in health were relatively rapid. These days it is much more common for people to live longer with multiple chronic conditions, and we have the technology to prolong life as death approaches. End-of-life care is fragmented, intensive, and costly — and patients’ wishes are often lost due to poor communication."
Read the complete article at: STAT
The diagnosis of a serious Illness. Important considerations to discuss with the Healthcare Team
Starting a Conversation with Your Healthcare Team
Whether you or a loved one have been newly diagnosed with a serious illness, or have been told your disease has progressed, you will have to make decisions about treatment. You may have many thoughts and emotions at this time. This can be a time of uncertainty and it is common to feel worried. It can be helpful to ask your healthcare team questions about what to expect, how to plan and what support and resources are available to you and your family.
It can be helpful to ask your healthcare team questions about your illness so that you can best understand your treatment options. The following is a list of questions that may help you to make informed decisions about your plan of care. Please ask these questions if they are helpful in guiding you and your family, or ask whatever questions are important to you. It can be helpful to bring your list of questions to your medical appointment and record/write down the answers. If you have the support available, you can have someone accompany you to your appointments to listen and help record the details.
Some questions you may ask your Healthcare Team:
• Is the condition short or long-term? Reversible or irreversible?
• Is the Illness curable or incurable?
• What types of treatment are available to treat the illness/condition?
• Where is this treatment offered? Hospital? Clinic? Home?
• What is the goal of treatment (cure, manage pain/symptoms, improve function, extend life)?
• If the goal of treatment is to extend-life, how long does the average person live while receiving this treatment? What about those who do not receive this treatment?
• How often is this treatment successful?
• Does having this illness/condition impact the effectiveness of treatments/
interventions one might receive in an Intensive Care Unit?
• What are the common risks and side effects of this treatment? Are there any possible dangers connected to this treatment?
• Where and how often will I receive this treatment? How long do you expect this treatment to continue?
• Is there a financial cost associated with this treatment?
• When and how will you know if these treatments are working?
• When or why might these treatments stop? If this treatment stops, what are other treatment options?
• How will this treatment impact my life? What are the expected physical, emotional, psychological and practical issues?
• What type of additional support is available to me? What about my family?
• What are the physical, emotional, psychological and practical resources that
can help? How do I/my family access them?
It is important to take time to have conversations about your treatment with your healthcare team. Please ask questions that are important to you. Honest and open communication about your healthcare is so essential.
The Conversation Placebo
"What’s often overlooked is that the simple conversation between doctor and patient can be as potent an analgesic as many treatments we prescribe."
How the United States Is Changing End of Life Care @attn
“As people live longer and medicine becomes more advanced, doctors have more ability than ever to hold off death. Yet many people put virtually no thought into whether they actually want their lives extended past a certain point — leading to a raft of unnecessary, unhelpful, and possibly unwanted medical procedures shortly before a person's death.”
When Patients Leave ‘Against Medical Advice’
"As physicians, we must explore our patients’ reasons for wanting to be discharged and have open and truthful conversations with them. We assume that keeping them in the hospital is always better for their health. But health encompasses the physical, mental and psychological.
In the end, my patient’s leaving was not about our therapeutic alliance. It was not about me at all. It was about her, the patient, as it should be."
LETTING GO: What should medicine do when it can’t save your life?
“People have concerns besides simply prolonging their lives. Surveys of patients with terminal illness find that their top priorities include, in addition to avoiding suffering, being with family, having the touch of others, being mentally aware, and not becoming a burden to others. Our system of technological medical care has utterly failed to meet these needs, and the cost of this failure is measured in far more than dollars. The hard question we face, then, is not how we can afford this system’s expense. It is how we can build a health-care system that will actually help dying patients achieve what’s most important to them at the end of their lives.”