“Thinking about death is frightening, but planning ahead is practical and leaves more room for peace of mind in our final days. In a solemn, thoughtful talk, Judy MacDonald Johnston shares 5 practices for planning for a good end of life.”
How to tell everyone what kind of #music to play at your #funeral. #ACP
“For Andrew Smith, a six-day stay in hospital got him thinking about life and death.
Granted, he was only having a toe removed. But what would happen if he passed away? Did his family know what kind of music he would want played at his funeral, or whom he would want in attendance?
‘I thought, I really need to get this stuff written down. But then I decided there’s a lot of people in the same situation as me, so if I can create a website where people can do it at home, at their own pace, that would be awesome,’ says the 44-year-old from Halifax who now lives in Vancouver.
The result of his thinking was Final Wish, a secure website that stores information that people would want shared at their time of passing. That includes what should be done with social media accounts and who should look after pets. Upon death, that information can be accessed by preappointed confidants.”
Are #Families Ready For The #Death And #Dying #Conversation? #ACP #InformedChoice
"The Institute of Medicine (IOM) believes the time is right for a national dialogue to normalize the emotions on death and dying. They think that the social trends point toward a growing willingness to share stories about the end-of-life care and that it will help drive more family discussions. In the IOM consensus report, Dying in America, experts found that accessibility of medical and social services could improve a patient’s life at the end. But if people don’t discuss which medical care or social services they want or not, how will their wishes be known and carried out?"
#Dying Better, Even If It Means Sooner. Delaying #death with excessive, expensive end-of-life care often does more harm than good.
"Looking back, many sons and daughters I have worked with regret having encouraged a parent to undergo a hip surgery. Spouses regret pushing for their loved ones to be intubated, and many patients struggle to balance the suffering with the life-prolonging effects of their treatments. Such regrets are the outgrowth of an approach to death that is focused on delaying death rather than being present and accompanying loved ones as they are dying. Accessing death-delaying treatments often comes at the expense of easing discomfort and being intentional about the nonmedical ways we can help our dying loved ones".
Why #Death Is Good Dinner #Conversation. #ACP @deathoverdinner @convoproject
"As I write this, I’m five years post-diagnosis and officially in “survivorship” care – I now go in for follow-up only once a year. And I have to admit, with cancer further and further in the rearview mirror, it’s easy to get back into denial mode when it comes to death – “I’m going to live forever!”
But we need to acknowledge death, talk about it, whether we’re a terminal patient, a just-diagnosed Stage I patient, or someone entering “survivorship.”
Recently, there have been the beginnings of a movement to help us all get real and have “the talk” about death.
So let’s get talking. Even if it’s scary and awkward, having this talk will greatly increase the chances that your end-of-life wishes are honored.
Death Over Dinner and The Conversation Project are organizing a week-long National Dinner Party to Dine and Discuss Death April 16 through 22".
How to Talk About Dying.
“Too many people we love had not died in the way they would choose. Too many survivors were left feeling depressed, guilty, uncertain whether they’d done the right thing.
The difference between a good death and a hard death often seemed to hinge essentially on whether someone’s wishes were expressed and respected. Whether they’d had a conversation about how they wanted to live toward the end…
We still need to transform the cultural norm from not talking about how we want to live at the end of life to talking about it. The real work to close the gap is not just for doctors and patients. It’s for mothers and daughters, husbands and wives, families and friends. We have to bring people to the kitchen table to talk with those they love to have the conversation. And to do this before there is a crisis. Not in the I.C.U.”
In #Palliative #Care, #Comfort is the Top Priority. #HPM
"Although 40 percent of their palliative care patients can expect to be cured, 'there clearly still are both patients and oncologists who have an inappropriate association in their minds,' he said. 'They still associate palliative care with giving up.'
To the contrary, palliative care can help patients live fully, regardless of their prognoses."
This is not Casualty – in real life #CPR is brutal and usually fails. #ACP #Awareness
"Modern medicine, however, still shies away from discussions about natural death and dying, and is more comfortable in the realms of what can be done. Doing something always trumps doing nothing. Healthcare professionals have become willing interventionists, and we cannot stop meddling, interfering and attempting to fix.
Many people I speak to presume that if the label “Not for CPR” or “DNACPR” (Do Not Attempt CPR) is added to their notes, this might preclude them from other resuscitative treatments such as antibiotics, fluids and blood transfusions. Dispelling this myth takes time and reassurance. Patients can still have active, resuscitative measures if they become increasingly unwell, but remain not for CPR for when their heart stops".
A thank you letter to David Bowie from a #Palliative #Care doctor
“So… to the conversation I had with the lady who had recently received the news that she had advanced cancer that had spread, and that she would probably not live much longer than a year or so. She talked about you and loved your music, but for some reason was not impressed by your Ziggy Stardust outfit (she was not sure whether you were a boy or a girl). She too, had memories of places and events for which you provided an idiosyncratic soundtrack. And then we talked about a good death, the dying moments and what these typically look like. And we talked about palliative care and how it can help. She told me about her mother’s and her father’s death, and that she wanted to be at home when things progressed, not in a hospital or emergency room, but that she’d happily transfer to the local hospice should her symptoms be too challenging to treat at home.
We both wondered who may have been around you when you took your last breath and whether anyone was holding your hand. I believe this was an aspect of the vision she had of her own dying moments that was of utmost importance to her, and you gave her a way of expressing this most personal longing to me, a relative stranger.
Thank you”.
Making a living will is a good idea. Telling people about it is even better. #HPM #ACP
Baby Boomers' Last Revolution Will Be Changing the Way We Die. #HPM
"Each person should have the chance to decide when it is time to shift from health care toward a cure to health care for comfort and pain management, as many doctors choose to do for themselves. That means giving us and our families the information and support they need. Death is not quick and simple, like in the movies. Just as they have learned to do with childbirth, health professionals need to learn to talk to patients and their families about what to expect. That knowledge provides reassurance and a sense of control. It is more important than any advanced directive or pain relief".
Patients aren’t told that death is near until too late. We can do better.
"Oncologists, cardiologists, and other specialists can often predict a patient’s rate of decline based on a specific disease, Obermeyer said. But patients, particularly those who are elderly, often suffer from more than one serious illness that make it more difficult to predict when they’re near death. So a pulmonologist might treat someone’s pneumonia, for instance, without recognizing it signals a broader decline".
"A parting lesson from my parents". ~Andrew Dreyfus
"As I have become more involved with this work, I have wondered whether the CEO of a large health plan is the right person to talk about end-of-life care. But I only have to remember how important this issue was to my brother and my parents to realize that — in this case at least — my personal experience should inform my professional actions. Everyone, regardless of economic, cultural, racial, or geographic differences, must have their choices and values heard and respected. Everyone deserves the chance to live the best life possible, to the very end".
Op-Ed 'I have terminal cancer. And I'm dying in a yearish.'
"I understand that my infinitesimally tiny piece in all this is coming to a close. Letting go will be difficult, but death has its own clock. So I will take solace in the idea that, once gone, I may come to occupy a small space in the hearts of the people who loved me most. And perhaps from there, I will be a source of a few simple reminders: Time is limited. Life is miraculous. And we are beautiful".
Dignity, Respect and Choice: Advance Care Planning for End of Life for People with Mental Illness.
"Dignity, Respect and Choice: Advance Care Planning for End of Life for People with Mental Illness is a two part resource that will help support people with mental illness, their families and carers, and health professionals with the complex issues which might arise around Advance Care Planning for End of Life".
Words to Live By...
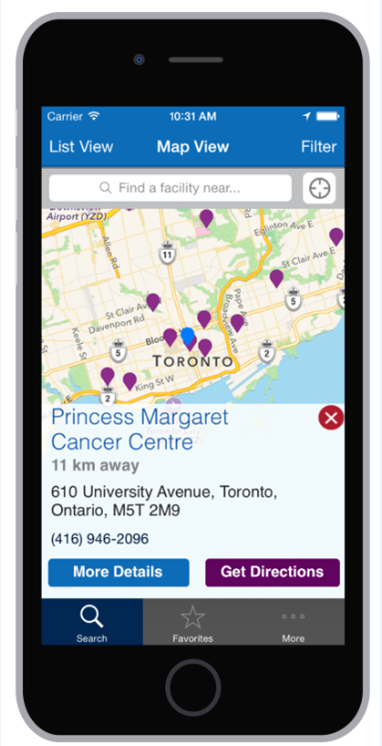
Inpatient Hospice Palliative Care Directory free via iOS and Android.
"Although some people hope to remain at home for the duration of their illness, many people find that admission to an inpatient setting can also be helpful. The inpatient care settings in the directory include palliative care units, residential hospices and dedicated palliative care beds within local hospitals. Inpatient hospice palliative care support includes 24 hour care, specialist pain and symptom management and psychosocial support for patients and families.
The map provides access to a directory which includes more information about inpatient hospice palliative care settings across Ontario. The list of facilities below may not be complete - there may be hospice palliative care settings which are not in the directory.
For contact information and details about the facility, click on a specific location. If you want more information, contact the hospice or palliative care program directly".
This App Will Help You Sort Through Your Views On Dying.
"There are apps for nearly everything -- ordering food, catching rides and finding dates, to name just a few of the common tasks people accomplish via a swipe of a screen. Now, a Boston-based company wants to make thinking about and planning for death just as simple.
Cake, as in “a piece of cake,” is a website and soon-to-launch app that asks people a series of yes-or-no questions about the end of their lives in order to help them think about certain issues, plans and needs. The topics include funeral preferences and financial planning, as well as whether there are places people want to see before dying and how satisfied they would be with their relationships if they died tomorrow.
'One of the biggest problems right now is that even if you want to have these conversations, most of us have no idea where to start. It's daunting and overwhelming,' Chen said.
'Even though we know ourselves, we may not truly understand our own values around end of life because most of us haven't spent much time thinking about it. We developed the app as a way to ease people into thinking about the end of life'.
The app is targeted toward users who want to talk about dying to their loved ones, as well as those who want to share their end-of life-wishes with their doctors and caretakers.
'We interviewed dozens of health care professionals and routinely heard doctors say that bringing up advance care planning ‘is the hardest part of my job.’ Even doctors who are trained in how to have these conversations find it challenging to bring up,' Chen said. 'Additionally, there's often not a lot of time at the doctor's office. It makes sense to provide a synchronous tools that empower people to think about things on their own and with their families while they're in the waiting room, or at home'.”
Best Endings. End of Life Planning Made Easier.
"It’s not just medical decision at end of life: we each have personal preferences. This often needs time and thought.
3 points to keep in mind:
- Thinking about your end-of-life can be exhausting and emotional.
- Thinking through what’s important often means having ‘Aha!’ moments about yourself.
- Determining personal choices at end of life can give you and yours peace of mind.
What’s important?
What to consider?
How much do I want to know?
You are The Boss"!