"One can only truly understand and appreciate life when faced with one’s own mortality. Nobody wants to talk about death, but it is one of the only things that is certain in life, so an awareness of this finitude allowed my family to take advantage of the time we had left together. “Cancer Family, Ongoing” is the story of family, looking at the experiences of two parents who were in parallel treatment for stage four cancer, side by side. The project looks at love and life in the face of death. It honors my parents’ memory by focusing on their strength and love, both individually and together, and shares the story of their final chapters, which came to a close just 364 days apart from one another."
Are #Families Ready For The #Death And #Dying #Conversation? #ACP #InformedChoice
"The Institute of Medicine (IOM) believes the time is right for a national dialogue to normalize the emotions on death and dying. They think that the social trends point toward a growing willingness to share stories about the end-of-life care and that it will help drive more family discussions. In the IOM consensus report, Dying in America, experts found that accessibility of medical and social services could improve a patient’s life at the end. But if people don’t discuss which medical care or social services they want or not, how will their wishes be known and carried out?"
The Meaning of #Life: #Palliative #Care Makes Every Moment Count. #hpm
"For someone facing a serious, chronic illness, the answers to that question take on a sharp focus. A patient with heart disease might want enough energy to walk around the neighborhood. A cancer survivor may want to feel like herself again after rounds of chemotherapy. Others might have a goal of seeing their children get married—or perhaps to get married themselves.
Helping patients get the most out of life is the aim of palliative care—which could surprise some people who associate the specialty with hospice, or care delivered in the final days and hours. Palliative care services do indeed benefit people nearing the end of their journey, but the field has become much broader over time. Many patients with a life-threatening disease now start receiving palliative care early—sometimes soon after diagnosis..."
On #Widower Watch. #hpm @otherspoon
"Marking family and personal occasions in this way has become increasingly important to all of us; these events intersect long, quiet weeks with laughter and company. And here’s the often unacknowledged benefit to keeping watch on a widower: With my grandparents dead and my friends all around my age, he diversifies my social life as much as I do his. He gives me a perspective on the city we live in that my peers simply don’t have. We spend our time together talking about our dissimilar lives and the things that matter to us, reminiscing about his many rich years, and looking up old poems in the vast library that lines the walls of his house. He is my friend and I miss him when I am away. As it turns out, nonagenarians are good company".
It’s worth it: #Love in the face of #Death. @lexibehrndt
"It’s a painful thing losing someone you love. It wrecks you at your very core. It shatters you, as they take a piece of your heart with them as they go. It is earth-shaking and dream-crushing and horrible in every way imaginable.
And it is worth every single second— every beat of their heart, every whispered prayer, every ounce of love given, every time you held their hand, every tear shed, every smile, every kiss, every lullaby and every single time they looked at you with soulful eyes, and told you in their own way, 'I love you, too.' They are worth it all.
Take it from me.
Choose the harder path. Love until you feel like your heart has given all it has, and then give a little more."
How to Tell Someone You’re #Terminally #Ill. #hpm
"Though everyone eventually dies, few know how to talk about the end of life. ‘‘People don’t know what to say,’’ Wanda says. ‘‘They’re afraid.’’ Be prepared for strange and stilted reactions. Some want to believe in a fix and will give you unsolicited health tips. (‘‘Don’t eat sugar.’’ ‘‘Avoid gluten.’’) You can ignore their suggestions but acknowledge the heart underlying them. People may offer to pray for you. ‘‘Prayers are good, but maybe what I need is someone to listen,’’ Wanda says. For that type of engaged listening, you may need to seek out a professional, like a trained social worker or a psychiatrist. Sometimes people who know about your condition — those you tell will tell others — will pretend your situation does not exist. Or weirder still, they will temporarily forget".
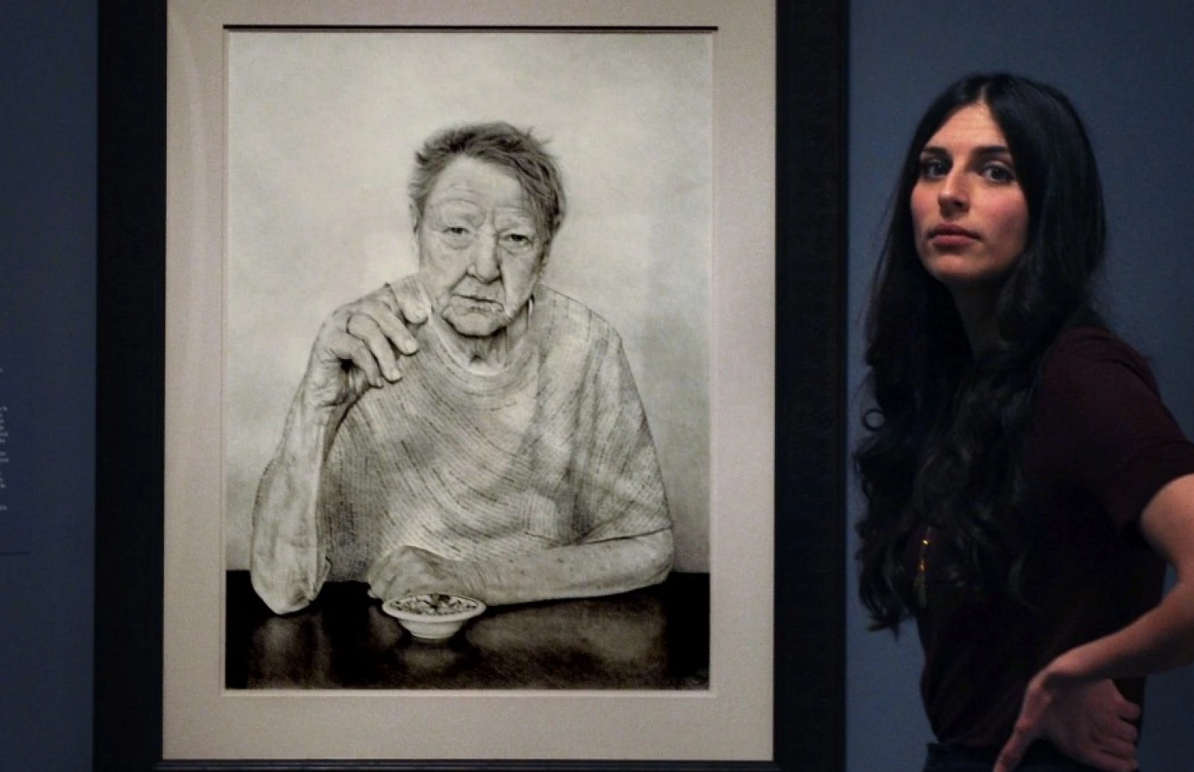
Drawing portraits of #dying people in #hospice taught this artist about #living. #hpm @claudiabicen
"Sitting in the museum’s atrium the day before the show opened, Biçen, 29, said she embarked on the project believing the dying might have lessons to teach her.
'Birth and death – these two moments of life are really sacred, and everything in between is kind of the madness of life,' she said. 'I thought that lying there on your deathbed you’re going to be confronting your life. What did it feel like to be dying? I think most people haven’t had a conversation with someone who is dying. It’s just pushed out of social consciousness and I think that’s problematic'."
How ‘Before I #Die’ Walls Boost #Palliative #Care. #hpm @candychang
" 'In order to die well, we need to learn how to talk about it,' Chang said, speaking to members of AAHPMN and HPNA.
Palliative care offers those with serious illnesses—both short and long term—more options with a focus on improving the quality of life. Public support for palliative care and end-of-life planning with medical professionals has swelled in recent years, but talking about death and care for those with serious illness is still complicated and difficult.
What Chang accomplished in her project was open up the conversations that are difficult to have—both with doctors and family members—whether under the circumstances of a serious illness or not. The chalkboards provided an anonymous outlet to share ideas, memories, anxieties and aspirations that are emotional and complicated."
Just Days Before Her #Father #Died, She Told Him What He Meant To Her. @NPR @StoryCorps
When he returned from the hospital to find hospice nurses awaiting him at his home, Eva says, he turned to her and said, "I think they think I'm gonna die."
And while he continued to get weaker as he approached the end of his life, Eva says she and her father had not spoken in depth about the prospect of his dying — until the conversation she recorded for StoryCorps.
"Do you think you're dying?" she asked him.
"Everybody dies," he replied.
"Are you afraid?"
"No."
"I wish it wasn't happening right now," she told him. "What are you most proud of, Daddy?"
"My kids."
"Your kids?"
"My family."
She did the interview with her father on a Tuesday afternoon. He died on Thursday night, that same week — on Jan. 29.
National #Family #Caregiver Day.
"On the first Tuesday of April, Canadians come together to recognize family members, friends, neighbours and other significant people who take on a caring role to support someone with a diminishing physical ability, a debilitating cognitive condition or a chronic life-limiting illness. Known as National Family Caregiver Day or National Carer Day, this special day encourages all Canadians to pay tribute and recognize the valuable contribution of family caregivers to our lives and our society as a whole."#Family
Compassionate Care Benefits. #Caregiver #Support #hpm
"Compassionate care benefits provide temporary income support to eligible individuals who must be away from work to provide care for a gravely ill family member at risk of death.
Effective January 3, 2016, the enhanced benefit, announced in 2015, allows claimants to collect up to 26 weeks of benefits, up from the current 6 weeks. Further, the period during which benefits can be taken is expanded to 52 weeks (up from 26 weeks). Benefits can be shared between family members.
Eligibility for compassionate care benefits remains the same, including the requirement for a medical certificate signed by a doctor attesting to the family member’s condition".
#Health Sentinel: Lack of #knowledge about #palliative care limiting its benefits to #patients, #hospitals. #hpm
"When Gerald’s physicians discussed options and next steps, palliative care was among them. Rozanne, a retired teacher, was familiar with hospice but unaware of palliative care as a specialized service.
'I didn’t have a clue,' she said, but added that through those services, 'our every need was met.'
Multiple studies show that, compared to awareness of hospice, “There’s significantly less familiarity with palliative care,” said Dr. Lyle Fettig, director of Indiana University School of Medicine’s Hospice and Palliative Medicine Fellowship program centered in Indianapolis…
Palliative care, according to the New York-based Center to Advance Palliative Care, is appropriate for any age individual and at any stage of a serious illness, whether that illness is cancer or a chronic condition, such as heart or lung disease. The goal is to improve quality of life for both patient and family through a holistic, interdisciplinary team approach”.
Embracing Life While In Palliative Care
"When you come to the end of your life, how do you mark it's last moments?
This short documentary,Embracing Life, aims to take away the stigma attached to death and dying.
Talking to patients in palliative care, the creators of the film enable conversations about how people feel about approaching the end of their life.
'The aim of the project has been to help build the capacity of communities to talk about death and dying, loss and grief, so that those living with a terminal disease can be better supported,' Sam Kelly from Calvary Health Care Bethlehem told The Huffington Post Australia.
The patients interviewed in this film give an incredibly positive perspective on what it's like to face death.
'Once I accepted that death was to come, I've just held everyday and I try to live it to the fullest,' said Tony Steele.
What Luck Means Now
"The day we learned the news, just 15 months had passed since our wedding on a New Hampshire hillside with friends and children gathered, fireworks exploding and a band backing us up as we performed a duet on a John Prine song and talked about the trips we would take, the olive trees we would plant. Each of us had been divorced almost 25 years. How lucky, everyone said, that we had found each other when we did.
Now, luck means having this operation. In four hours, luck will mean getting a call from a nurse who says: 'They’ve reached the tumor. They’re going in for it'."
Repeat After Me: 'Hospice Means More Care, Not Less.'
"If you or anyone you know has advanced illness that isn't meaningfully getting better (or keeps getting worse) in spite of many treatments and hospital stays and doctors' visits then you owe it to yourself to learn more about hospice sooner rather than later. This is especially true for more frail elders with serious illness because the hazards of additional hospitalizations and certain treatment side effects are more serious and more common. Ideally, hospice care is set up on a better day, in advance of a true crisis so that the hospice team and person receiving services can get to know one another and set up truly personalized care. Too many people elect hospice so late in their course of illness that they miss out on many of the benefits".
I'm Trying to Die Here. ~ Rev. Dr. Carla Cheatham
"Our goal is to maximize quality of life for whatever quantity naturally remains for everyone involved. Knowing that we are the interlopers, we strive to adapt to the personality and culture of the person receiving hospice as well as that of their entire family. We pay attention. We listen to stories. We pick up queues and share them with our team members so we can all work to provide as little intrusion as possible as guests in the home (whether “home” is one’s own or a room in a facility)".
In #Palliative #Care, #Comfort is the Top Priority. #HPM
"Although 40 percent of their palliative care patients can expect to be cured, 'there clearly still are both patients and oncologists who have an inappropriate association in their minds,' he said. 'They still associate palliative care with giving up.'
To the contrary, palliative care can help patients live fully, regardless of their prognoses."
When Your Loved One Is Ready for #Hospice Care - and You Aren't. #HPM
“And I had a lot of questions about hospice care, including whether I could stop it if I changed my mind later. (He told me I could stop it at any time, for any reason, and that if I changed my mind again I could resume the services.) The conversation was incredibly stressful. At one point I realized I was holding my breath.
After answering all my questions, Doug looked at me kindly and said, ‘You know, Marie, the real question for the caregiver is how to help the patient have the highest possible quality of life in the time that is remaining.’
That completely changed my thinking about the situation. It gave me a new and positive goal - to bring Ed as much happiness as possible. It led me to think about all the special things I could do for Ed -- visiting him more often, taking my little Shih Tzu to see him, having that violinist come back and play another concert, reading to him from the newspaper, and buying him even more of the stuffed animals he loved so much.”
A New Vision for Dreams of the #Dying. #eolc #hpm
"Dr. William Breitbart, chairman of the psychiatry department at Memorial Sloan Kettering Cancer Center, who has written about delirium and palliative care, said that a team’s response must also consider bedside caregivers: “These dreams or visions can be interpreted by family members as comforting, linking them to the legacy of their ancestry.
But if people don’t believe that, they can be distressed. ‘My mother is hallucinating and seeing dead people. Do something about it!’ Dr. Breitbart trains staff to respect the families’ beliefs and help them understand the complexities of delirium.
Some dream episodes occur during what is known as 'mixed-state sleep' — when the boundaries between wakefulness and sleep become fragmented, said Dr. Carlos H. Schenck, a psychiatrist and sleep expert at the University of Minnesota Medical School. Jessica Stone, the teenager with Ewing’s sarcoma, spoke movingly about a dream of her dead dog, Shadow. When she awoke, she said, she saw his long, dark shape alongside her bed.
Dr. Banas, the neurologist, favors the phrase end-of-life experiences. 'I try to normalize it for the family, because how they perceive it can push them away from that bedside or bring them closer,' she said."
"I See Dead People". #Dreams and #Visions of the #Dying.
"Dr. Christopher W. Kerr is the Chief Medical Officer at The Center for Hospice and Palliative Care, where he has worked since 1999. His background in research has evolved from bench science towards the human experience of illness as witnessed from the bedside, specifically patients’ dreams and visions at the end of life. Although medically ignored, these near universal experiences often provide comfort and meaning as well as insight into the life led and the death anticipated".