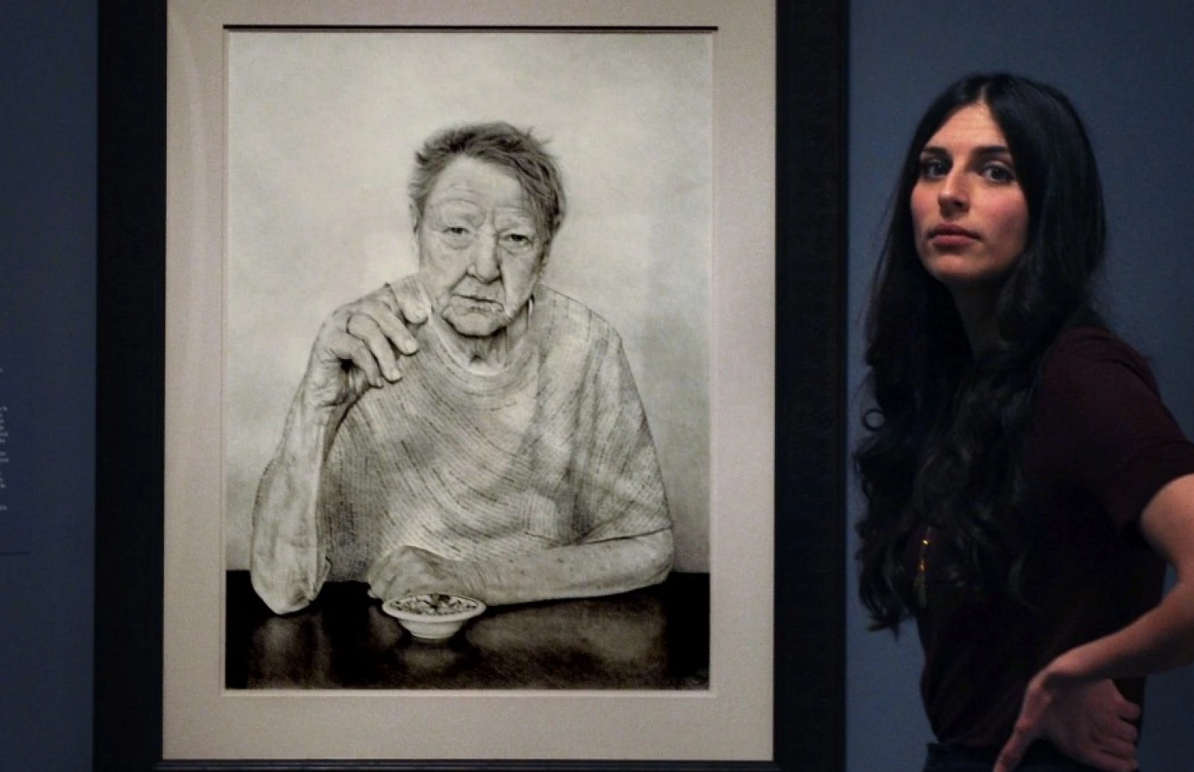
“In the early moments of critical illness, the choices seem relatively simple, the stakes high – you live or you die. But the chronically critically ill inhabit a kind of in-between purgatory state, all uncertainty and lingering. How do we explain this to families just as they breathe a sigh of relief that their loved one hasn’t died? Should we use the words “chronic critical illness”? Would it change any decisions if we were to do so? Here, I find that I am often at a loss.
I was quiet on the other end of the phone line that night. Was my patient stable? For the moment, she was. But with each event like this one, and there would be more, my patient would move further from the hope of ever reclaiming that life she had had in the fall: living in her own home, watching movies, cooking. I felt that I could see the weeks and months spooling out, a moment of calm, a new emergency. But this wasn’t the time to tell her daughter, not on the phone, not tonight.
And so I told her the truth – one truth, at least. Her mother was critically ill, but stable for the night”.