I am honoured to be co-presenting “Practical Tips: Lessons from the Front Line”, the final session in the National Community-Based Primary Palliative Care Community of Practice (CoP) series. This Continuing Professional Development is FREE for all health care professionals is part of The Palliative Care ECHO Project led by Pallium Canada.
This community of practice focuses on supporting primary care clinicians to integrate primary palliative care in their practices. It is geared towards interprofessional primary health care providers across Canada. Each session is accredited by the College of Family Physicians of Canada.
This is the final session in the second series, which includes 11 sessions taking place on a bi-weekly basis. All webinars are recorded and available for playback. Topics include:
Pain: Beyond the Basics: November 9, 2022
Communication: Part 1: November 23, 2022
Communication: Part 2: December 7, 2022
Palliative Care and Substance Use Disorders: January 18, 2023
GI Symptoms in Palliative Care: February 1, 2023
Delirium: February 15, 2023
Spiritual Care and Rituals Around Death and Dying: March 1, 2023
Palliative Sedation: March 15, 2023
Grief and Bereavement: Beyond the Basics: April 12, 2023
Practical Tips: Lessons from the Front Line: April 26, 2023 from 1–2:00 p.m. ET
Interested in becoming a part of this FREE COP? Visit The Palliative Care ECHO Project
Planning for My Care: Proud, Prepared & Protected
April 16th is National Advance Care Planning Day in Canada
Planning for My Care part of Proud, Prepared & Protected is a FREE booklet focusing on care conversations 2SLGBTQ+ people and healthcare providers to start conversations about values, wishes and concerns to help identify who you would want to make decisions, your Substitute Decision Maker (SDM) on your behalf should you not be able to make decisions for yourself.
Access FREE via https://www.virtualhospice.ca/2SLGBTQ/media/igkp01nf/2slgbtq-planning-for-my-care.pdf
Many who are 2SLGBTQ+ have experienced or witnessed discrimination and ignorance in a healthcare setting. You may have received inappropriate care or, even worse, been denied care. Some healthcare workers are not aware of the challenges the 2SLGBTQ+ communities face.
This document, focusing on care conversations for Two-Spirit and Lesbian, Gay, Bisexual, Trans, Queer, and all sexual and gender-diverse people, is intended to help you think about what is important to you, concerns you might have, and who you would want to make decisions for you if a time comes when you can’t make decisions for yourself.
Consider giving a copy of this document to the important people in your life, and sharing this information with healthcare providers. Take it with you when you attend appointments, call 911, visit the emergency department, or access other healthcare services. If your province or territory has a process for documenting your wishes for care, ensure this information is included on those documents and kept in the same place.
Source: Canadian Virtual Hospice
ADDITIONAL RESOURCES:
For more information on advanced illness, advance care planning, palliative care, end-of-life care and grief, please visit:
Canadian Virtual Hospice www.virtualhospice.ca
Advance Care Planning Canada values a free, accessible and open shared knowledge amongst the community. The website provides you with all the necessary tools to inform yourself on the most recent advanced care planning updates and developments. For more information and FREE resources, visist: https://www.advancecareplanning.ca/
FREE Advance Care Planning (ACP) workbooks
April 16th is National Advance Care Planning Day in Canada
“If Not You, Who? Who would you trust to make your healthcare decisions? Planning for your future healthcare needs is important. So, we’re asking: Do you know what would happen if you couldn’t speak for yourself? Who would you trust to make those #healthcare decisions for you?
You have the power to choose who that person is. They can be a family member, a friend, or anyone in your life that you trust to make the kinds of healthcare decisions you would want.
Think about who you would trust with making those important decisions for you.
Think about what matters most in your life and how that might help guide someone in making the kinds of healthcare decisions you would want.
The best time to think about this is now when you can speak for yourself. We have useful guides to help you along the way.
Choosing a Substitute Decision-Maker (SDM)
Advance Care Planning policies can vary dependent on your province or territory. In order to ensure your end of life wishes are honoured it is crucial to have an understanding of your province or territory policies. This includes understanding what your #rights and #privileges are, as well as understanding the laws and regulations regarding end of life care, specific to your province or territory. While creating your advance care plan it is also important to make sure that you are using the correct documents for your province or territory.
Who do you trust most to make decisions for your health care that follow your wishes?
Would that person be comfortable with making important decisions about your health quickly or in an emergency?
Have you spoken to them about what matters most in your life? When someone knows what you value most in your life, they can make more informed decisions about your health care.
What Matters Most? What does a good day look like for you?
What situations do you find difficult?
What gives you strength in difficult times?
What spiritual, cultural or religious beliefs, practices, or ceremonies are important to you?
What do you value more: the possibility of a longer life, or the possibility of a better quality of life?
These questions can help guide you and your substitute decision-maker and assist them to prioritize what matters most to you when weighing care options.
April 16th is Advance Care Planning Day. So, ask yourself: If not you, who?”
Source: Advance Care Planning Canada
There are multiple FREE Advance Care Planning (ACP) workbooks, toolkits and guides specifically created to follow the provincial/territorial requirements for your advance care plan. Visit for FREE FREE Advance Care Planning (ACP) resources across Canada https://www.advancecareplanning.ca/acp-across-canada/
April 16th is National Advance Care Planning Day in Canada.
It’s about conversations. It’s about wishes. It’s how we care for each other.
Advance Care Planning is about having conversations with family and friends, especially your Substitute Decision Maker – the person who will speak for you if you cannot speak for yourself in case of a health emergency. It may also include writing down your wishes, and talking with healthcare providers and financial or legal professionals.
Advance care planning is a process of reflection and communication, a time for you to reflect on your values and wishes, and to let others know your future health and personal care preferences in the event that you are unable to consent or refuse treatment or other care.
Think about what is most important to you – your values, wishes and beliefs.
Learn about your overall health. This may include current conditions you want to better understand.
Decide on your Substitute Decision Maker(s), one or more people who are willing and able to speak, for you if you cannot speak for yourself.
Talk about your values, beliefs and wishes with your Substitute Decision Maker(s), family, friends and health care providers.
Record your values, wishes and beliefs in your Advance Care Planning Guide, in a letter, poem, video or audio recording.
Source: Advance Care Planning Canada
ADDITIONAL RESOURCES:
For more information on advanced illness, advance care planning, palliative care, end-of-life care and grief, please visit:
Canadian Virtual Hospice www.virtualhospice.ca
Living My Culture www.livingmyculture.ca
Advance Care Planning Canada values a free, accessible and open shared knowledge amongst the community. The website provides you with all the necessary tools to inform yourself on the most recent advanced care planning updates and developments. For more information and FREE resources, visit: https://www.advancecareplanning.ca/
National Caregiver Day is the first Tuesday of April in Canada.
“More than 8 million family and friend caregivers in Canada are providing care in the home. Most caregivers will feel unprepared and overwhelmed at some point. If you are caring for someone who is ill or living with mobility challenges, these modules are for you.
Access them anytime of the day or night, as many times as you need, and at no cost (FREE) via https://www.virtualhospice.ca/caregiving/
These modules include useful information, strategies, and suggestions for preparing for and providing care as illness advances:
-Strategiesfor difficult conversations
-Video demonstrations of caregiving tasks
-Guidance for recognizing and managing symptoms
-Suggestions for accessing programs and services
-Ways to care for yourself
Content is arranged in chapters and pages. Click a Chapter to see the pages and topics covered. You can move through the module pages using the list on the left-hand side or using the arrows at the bottom of the page. To return to the home page click the logo at the top left of the screen. Some modules include video clips showing how to do caregiving tasks or people sharing their experiences.”
Source: Canadian Virtual Hospice
If you have questions, email info@virtualhospice.ca
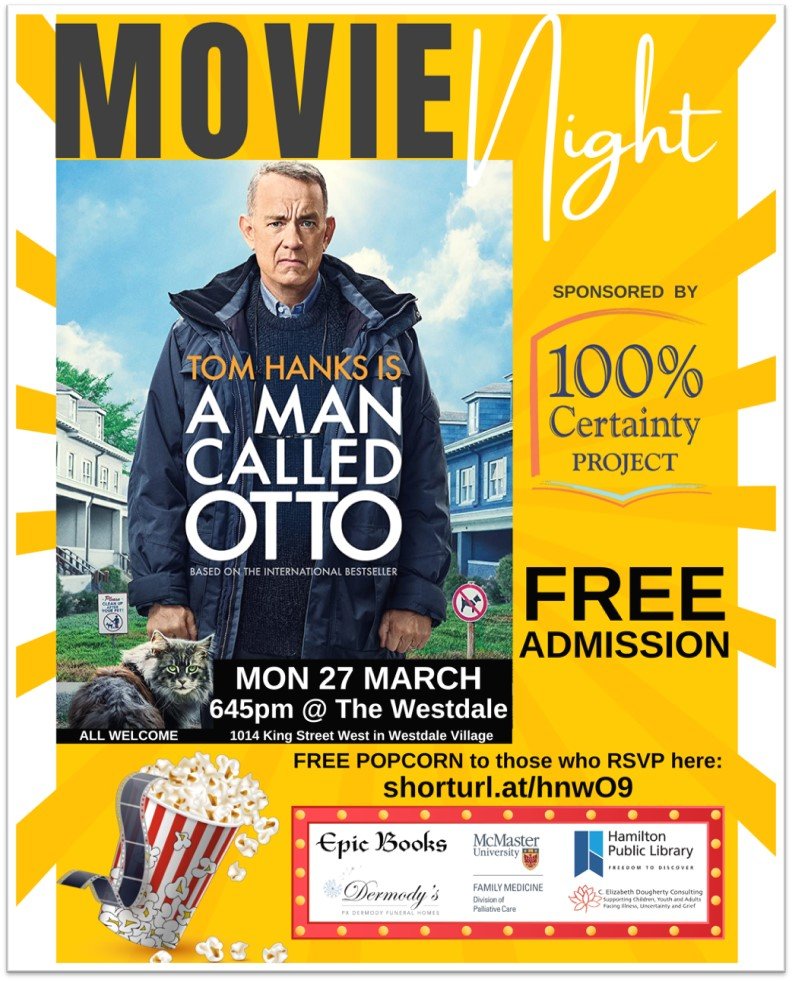
The 100% Certainty Project: FREE Event
I am honoured to be a member of both The 100% Certainty Project and the Division of Palliative Care at McMaster University.
The 100% Certainty Project, in partnership with Epic Books, PX Dermody Funeral Homes and the Hamilton Public Library, advocates that issues of #death, #dying, #grief and #bereavement need to be “reclaimed” by the community - by private citizens who are accustomed to end-of-life care being provided by our #healthcare system.
The 100% Certainty Project is hosting a FREE MOVIE at The Westdale Theatre in #HamOnt on Monday, March 27th (6:45pm). JOIN US in the beautifully renovated historic Westdale Theatre as we view the film (based on the #1 New York Times bestseller A Man Called Ove, a previous 100% Certainty Project book selection). This celebration-of-life story is a major motion picture starring Tom Hanks!
“Meet Ove (a.k.a. Otto) - the kind of man who points at people he dislikes as if they were burglars caught outside his bedroom window. He has staunch principles, strict routines, and a short fuse. People call him “the bitter neighbor from hell.” But must Ove be bitter just because he doesn’t walk around with a smile plastered to his face all the time?
Behind the cranky exterior there is a story and a #sadness. So when one November morning a chatty young couple with two chatty young daughters move in next door and accidentally flatten Ove’s mailbox, it is the lead-in to a comical and heartwarming tale of unkempt cats, unexpected friendship, and the ancient art of backing up a U-Haul. All of which will change one cranky old man and a local residents’ association to their very foundations.
Fredrik Backman’s beloved first novel about the angry old man next door is a thoughtful exploration of the profound #impact one life has on countless others.” (source: Simon & Schuster)
REGISTRATION IS REQUIRED ON EVENTBRITE via https://www.eventbrite.ca/e/a-man-called-otto-free-screening-tickets-581260484757
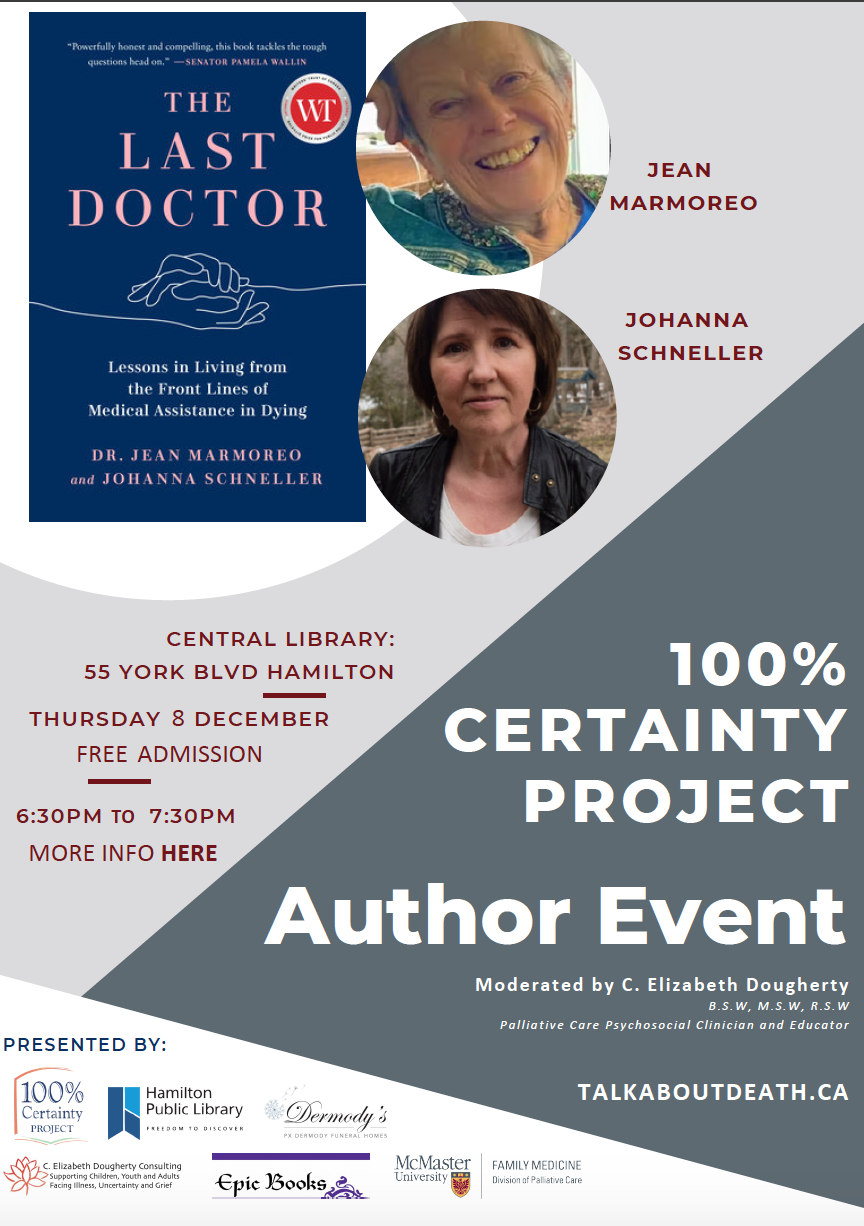
The Last Doctor: Free Public Event - December 8th
I am sharing this free Author Event as a part of the 100% Certainty Project, for The Last Doctor at the Hamilton Public Library on Thursday December 8th.
I am honoured to be moderating this discussion with the co-authors of The Last Doctor, Dr. Jean Marmoreo and Johanna Schneller, as we discuss their new book. At a time when end-of-life care and its quality are more in the public eye than ever before, The Last Doctor provides an accessible personal, deeply humane, and authoritative guide through this difficult subject.
Jean is a doctor, writer, advocate, athlete, and adventurer. She is a specialist in end-of-life medicine and was one of the first doctors in Canada to provide MAiD—Medical Assistance in Dying— when it became legal in 2016. Jean was a regular columnist for The Globe and Mail and The National Post.
Johanna is one of North America’s leading freelance journalists, specializing in entertainment features. Her cover stories have appeared in Vanity Fair, InStyle, Premiere, More, and Ladies Home Journal. Johanna co-wrote the bestselling book Uncontrollable with Mark Towhey and Woman Enough with Kristen Worley
Join us for a chat with the co-authors of The Last Doctor: Lessons in Living from the Front Lines of Medical Assistance in Dying. For information, please visit: https://events.hpl.ca/event/7549953
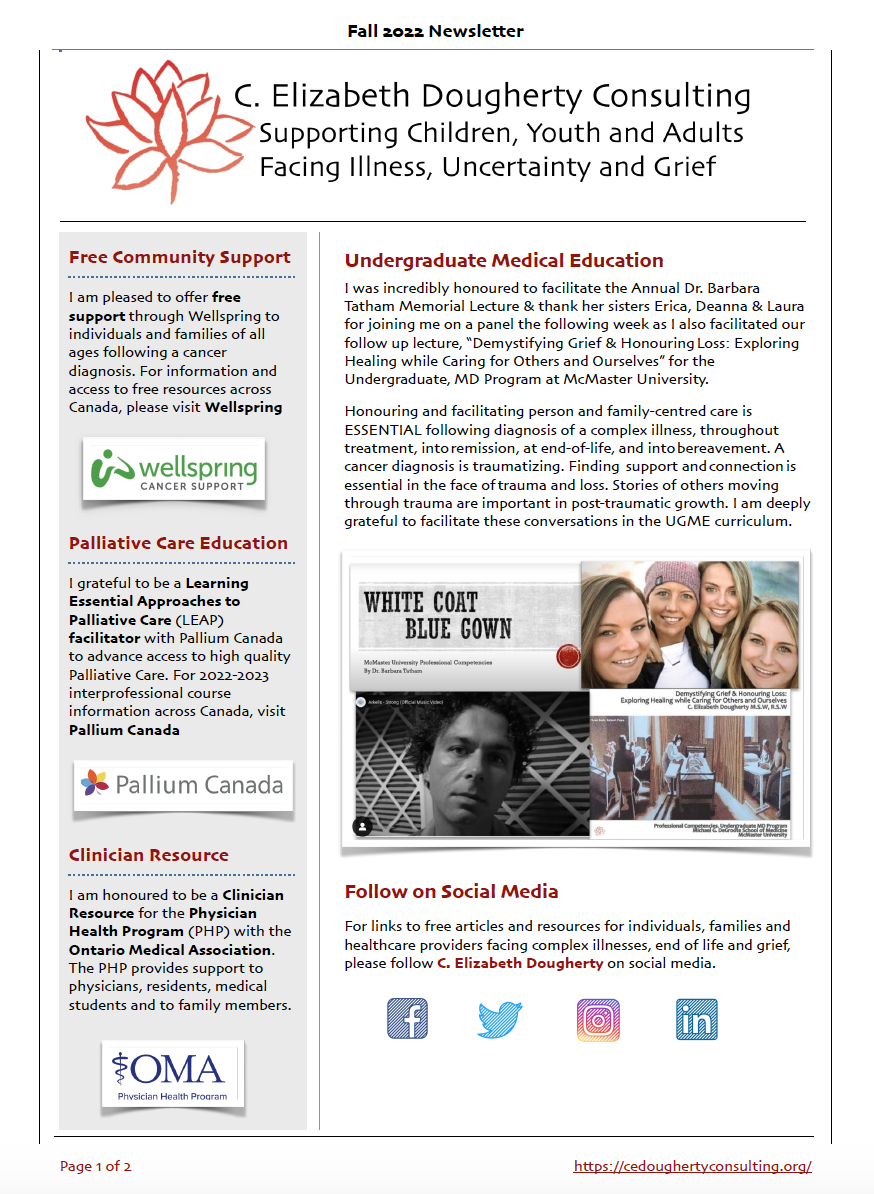
C. Elizabeth Dougherty Consulting Newsletter: Fall 2022
I am pleased to share my Fall 2022 Newsletter highlighting educational opportunities and my clinical work serving individuals, families, and healthcare providers facing complex illnesses, uncertainty and grief.
Medical Education: Honouring life, love, loss and legacy at McMaster University
Incredibly honoured to facilitate the Annual Dr. Barbara Tatham Memorial Lecture & thank her sisters Erica, Deanna & Laura for joining us to demystify grief, honour loss & explore healing while caring for others and ourselves. Honouring Dr. Tatham's life, legacy and brilliant contributions to Medical Education at McMaster University.
Honouring person and family-centred care is ESSENTIAL from time of diagnosis, throughout treatment, into remission, at end-of-life, and into bereavement.
A cancer diagnosis is traumatizing. Finding community, support and connection is essential in the face of trauma. Stories of others moving through trauma are always important in post-traumatic growth (Tedeschi & Calhoun). Strength is often correlated, almost paradoxically, following an increased sense of being vulnerable - of being human.
Today, please take a moment to connect with your breath, honour your strengths and make space for who and what matters most in your life. ❤️
Today is the Annual #TerryFoxRun. To support Dr. Tatham's life, legacy and indomitable spirit in the face of cancer, please donate to #TeamBarb https://run.terryfox.ca/team/teambarb
C. Elizabeth Dougherty Consulting Spring Newsletter
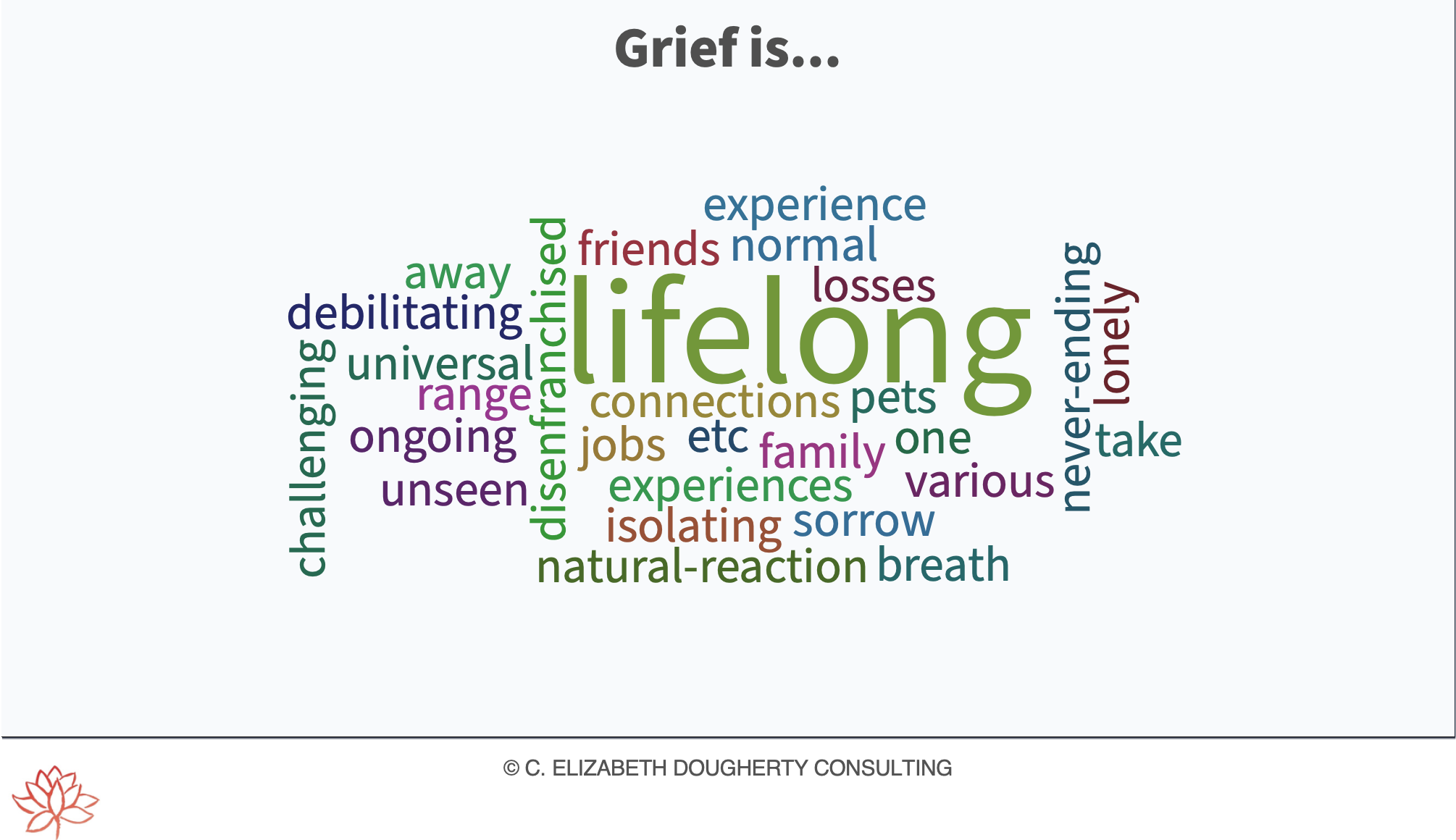
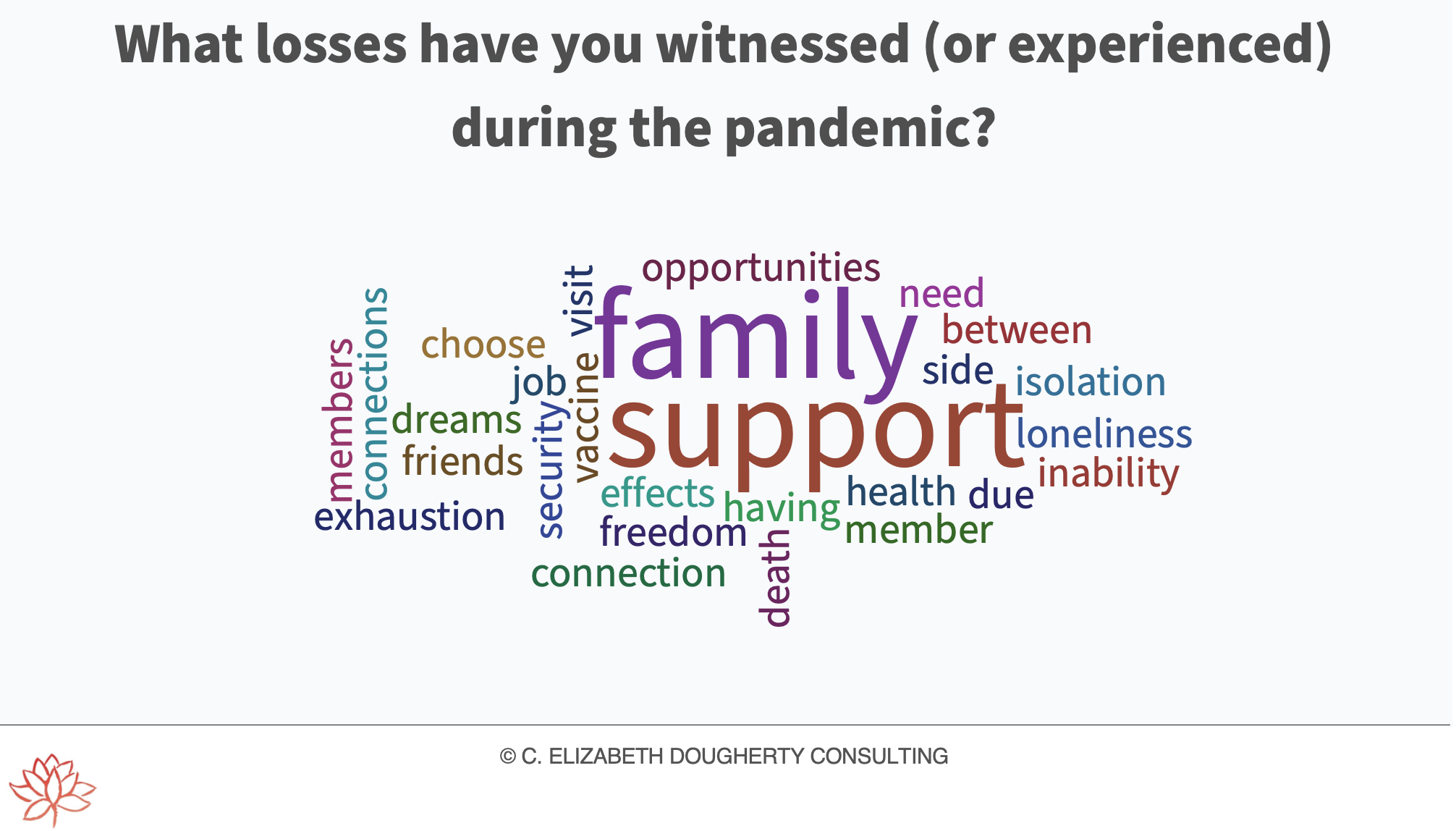
Loss in the Time of COVID: Exploring the Impact of Grief
Honoured to deliver Loss in the Time of COVID: Exploring the Impact of Grief as the Keynote address at Trillium Health Partners in support of National Hospice Palliative Care Week in Canada.
My sincere gratitude to everyone who joined our discussion via Zoom, for sharing time, reflections and energy - and for acknowledging the impact of trauma, loss and grief for healthcare providers as we continue to serve so many facing trauma, loss and grief during the pandemic.
Best Oral Paper Award at #HPCO2022!
Incredibly honoured as the Clinical Lead to receive the Best Oral Paper Award at #HPCO2022 Hospice Palliative Care Ontario Annual Provincial Conference with our incredible interprofessional team: Ann Vander Berg, Allyson Oliphant, and champion for our project - Dr. Andrea Folic for "Care Beyond Walls: Innovation, Implementation and Evaluation of a Medical Assistance in Dying-Specific Bereavement Support Group for Caregivers"
Exploring the Role of Social Work in Palliative Care
So grateful to speak with my friends and colleagues Drs. Hsien Seow and Sammy Winemaker on their podcast The Waiting Room Revolution.
We explored the role of Social Work in Palliative Care, the value of proactive and compassionate person and family-centred support following diagnosis of any serious illness, exploring loss and grief through to end-of-life and bereavement, creating space for essential conversations, and the healing power of silence.
Follow their podcast for essential tips and tools to navigate the healthcare system following diagnosis of a serious illness. To listen to our conversation, click here
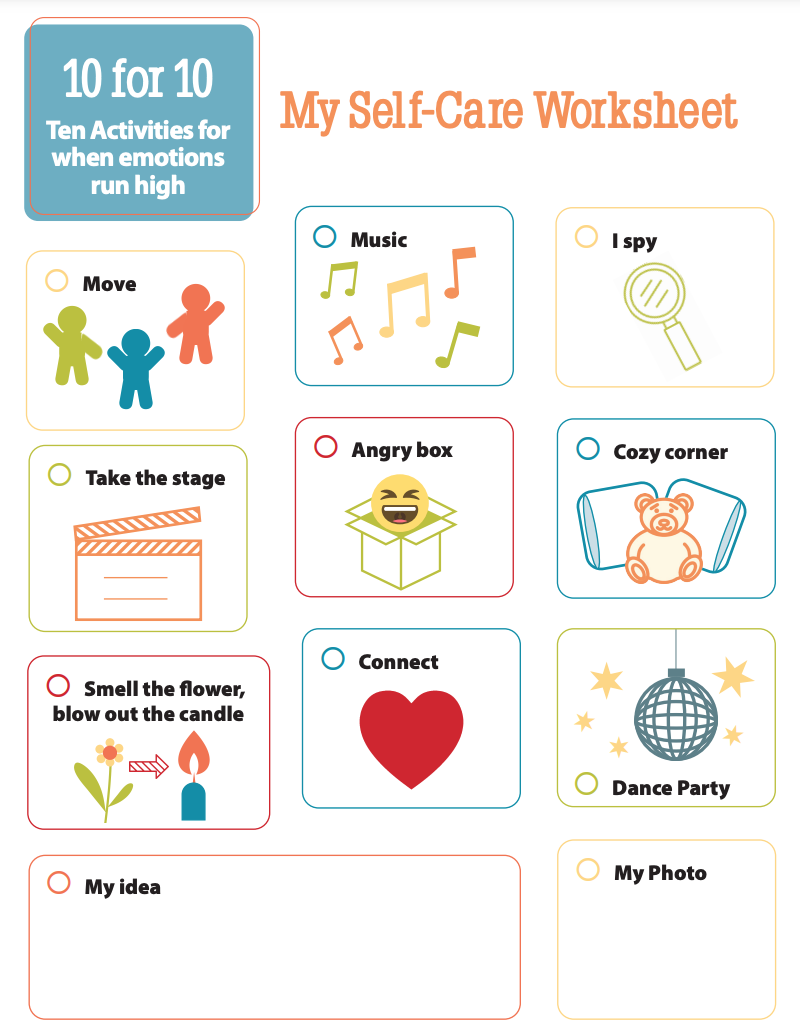
10 for 10: Ten Activities for when emotions run high
10 for 10: Ten Activities for when emotions run high via NACG The Dougy Center & KinderCare
Parents and Caregivers, you can encourage use of this worksheet in a few different ways:
Children and teens can use it to choose any activity when their emotions are running high (a supportive reaction).
You can ask them to refer to it regularly and choose self-care activities at any time (a proactive response).
Children or teens can mark off the activities they do throughout the day/week (promoting a sense of accomplishment).
They can create and choose their own activity to help self-regulate (encouraging self-compassion & creativity).
They can also design their own self-care worksheet (exploring empowerment).
Source: https://childrengrieve.org/12-resource/309-resources-2
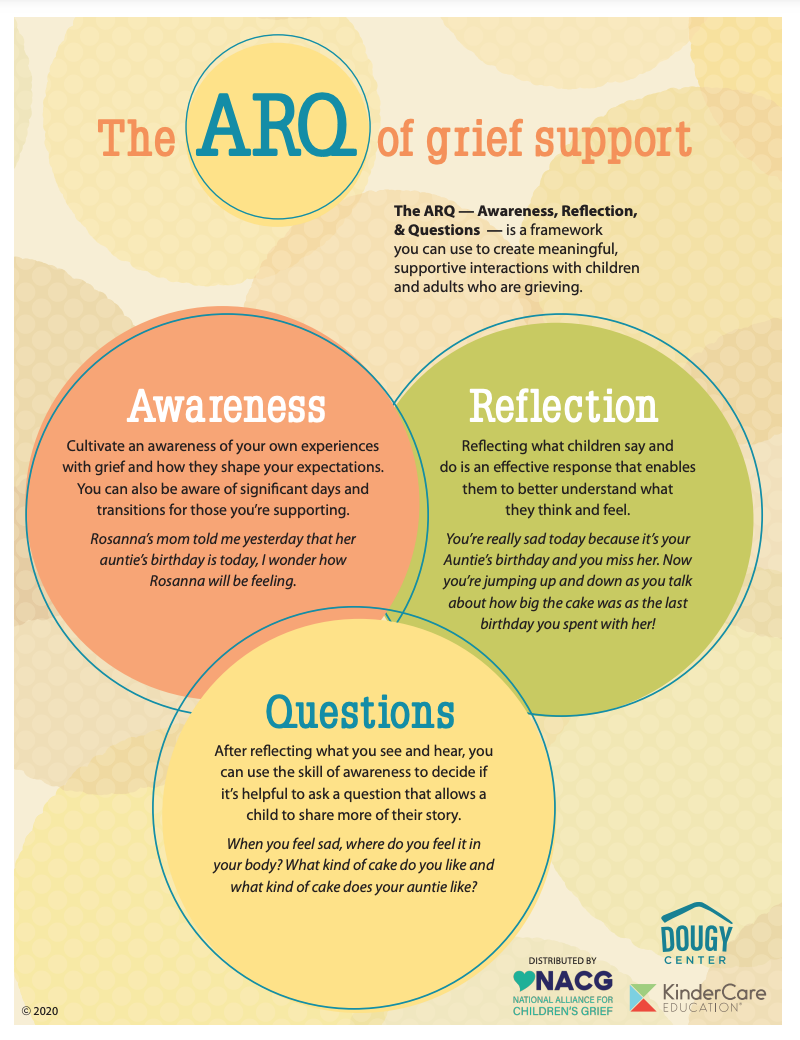
The ARQ of Grief Support
The ARQ of Grief Support:
Awareness
Reflection
Questions
The ARQ of Grief Support via NACG, The Dougy Center & KinderCare is a framework you can use to create meaningful, supportive interactions with children, teens and adults facing grief, loss & grieving
Source: https://childrengrieve.org/12-resource/309-resources-2
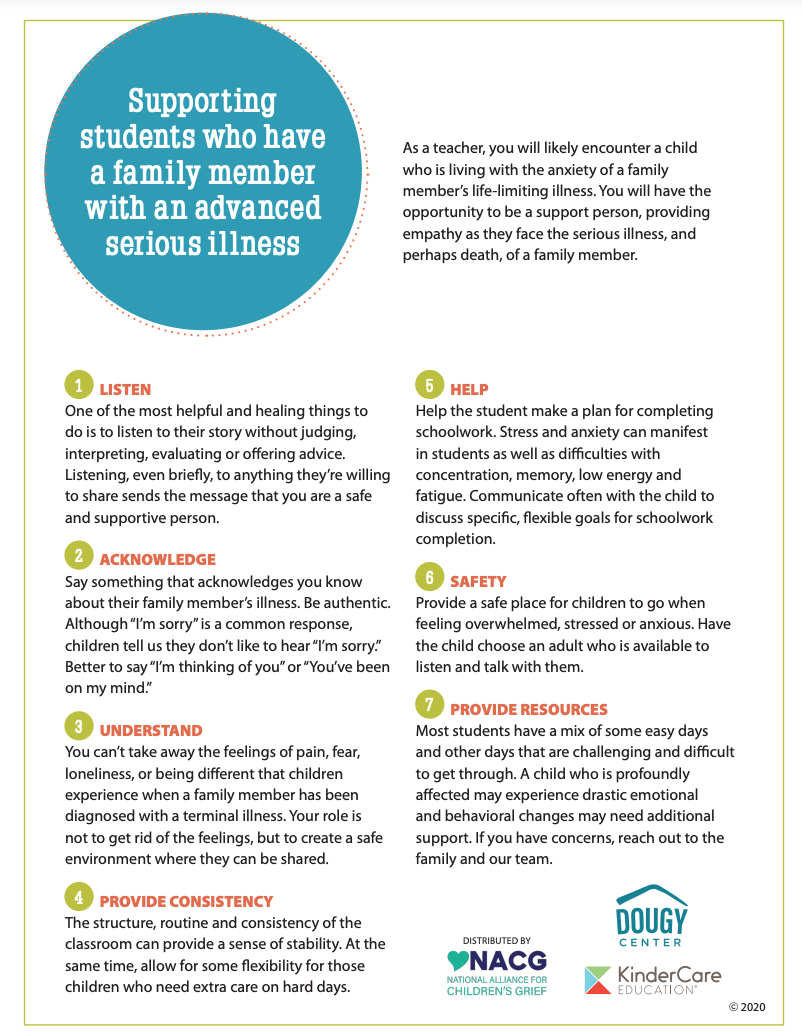
Supporting children and youth who have a family member with an advanced serious illness
Supporting children and youth who have a family member with an advanced serious illness via NACG The Dougy Center & KinderCare
At some point, we all encounter a child or teen who is living with the anxiety of a family member’s life-limiting illness. You can have the opportunity to be a support person, providing empathy as they face the serious illness, grief, loss and perhaps death, of a family member.
Some considerations include: Listen, Acknowledge, Understand, Provide Consistency, Help, Safety, Provide Resources
Source: https://childrengrieve.org/12-resource/309-resources-2
C. Elizabeth Dougherty Consulting - Winter 2022 Newsletter
I am honoured to share my winter 2022 newsletter with free resources for individuals and families of all ages facing a complex illness, following diagnosis through to bereavement.
I am also grateful to also share teaching experiences including: undergraduate and graduate Social Work Education; undergraduate interdisciplinary education; and Interprofessional Education for healthcare providers and volunteers exploring informed conversations, honouring person and family-centred care, demystifying grief, and advocating for high-quality palliative care.
Join the movement to #UnderstandGrief
Join the #UnderstandGrief movement! Here's how:
1. Advocate that grief is not a mental disorder; our social and cultural context impacts how we grieve. Question the narrative of “mental disorders” and consider all the factors that can contribute to how a person responds to the death of someone in their lives.
2. Consider the language you use and how it can impact people. People who are grieving often receive patronizing responses to “move on” or “find closure” when what they need most is to feel understood.
3. Educate others about being grief-informed. Share the 10 core principles of being grief-informed.
4. Broaden the dialogue about the need for diversity and inclusivity in grief research and support. We need to reach beyond limited and narrow perspectives to understand and support how grief is experienced by people of different beliefs, cultures, ethnicities, backgrounds, abilities, and experiences.
5. Challenge myths about grief. Grief doesn’t follow an orderly path. When someone is grieving, don’t impose expectations on them about how they should feel or respond, or how long their grief should last. Every experience of loss is different.
6. Acknowledge and address the injustices of labels. Rather than labeling people who are grieving with a mental disorder, consider framing the challenges we face when we’re grieving as just that: challenges we experience when coping with the death of someone in our lives.
7. Recognize and acknowledge that every experience of loss is a unique experience. People will likely respond to the death of each person in their life differently because every relationship is unique.
8. Strengthen relational connections. We need connections with others who are understanding and compassionate, especially when difficult and painful things happen.
9. Honour lived experience. To honour the lived experience of others involves offering the gift of nonjudgmental listening, open mindedness, and support.
10. Be compassionate with yourself and with others. One of the ways we can “walk our talk” is to demonstrate the same compassion toward ourselves that we hope others will have for themselves, particularly when we’re grieving.
Via The Dougy Center
What to say (and NOT to say) when someone is grieving
Most don't know what to say when someone is grieving. Here are some suggestions to offer a grieving parent, caregiver, or colleague. These questions can also be adapted for children.
via National Alliance for Grieving Children, The Dougy Center and KinderCare Education
C. Elizabeth Dougherty Consulting - Fall 2021 Newsletter
I am honoured to share my Fall 2021 newsletter including resources for individuals and families of all ages facing a complex illness, following diagnosis through to bereavement. I am also grateful to also share my teaching experiences including: undergraduate and graduate Social Work Education; undergraduate Medical Education; and Interprofessional Education for healthcare providers exploring informed conversations, honouring person and family-centred care, demystifying grief, and advocating for palliative care.