“How we die is regularly in the headlines as we await government legislation to be tabled in response to the 2015 Supreme Court of Canada decision legalizing physician-assisted dying. Palliative care gets less attention, but it is what most of us will want at the end of life: drugs to relieve agitation, pain, agonal breathing and other symptoms. Nurses can provide soothing medications, but only after doctors have issued prescriptions, often with increasing dosages. But as the Crosbie family discovered, doctors are few and far between in long-term care facilities, especially on weekends. Their experience is a cautionary tale.”
Are #Families Ready For The #Death And #Dying #Conversation? #ACP #InformedChoice
"The Institute of Medicine (IOM) believes the time is right for a national dialogue to normalize the emotions on death and dying. They think that the social trends point toward a growing willingness to share stories about the end-of-life care and that it will help drive more family discussions. In the IOM consensus report, Dying in America, experts found that accessibility of medical and social services could improve a patient’s life at the end. But if people don’t discuss which medical care or social services they want or not, how will their wishes be known and carried out?"
The Meaning of #Life: #Palliative #Care Makes Every Moment Count. #hpm
"For someone facing a serious, chronic illness, the answers to that question take on a sharp focus. A patient with heart disease might want enough energy to walk around the neighborhood. A cancer survivor may want to feel like herself again after rounds of chemotherapy. Others might have a goal of seeing their children get married—or perhaps to get married themselves.
Helping patients get the most out of life is the aim of palliative care—which could surprise some people who associate the specialty with hospice, or care delivered in the final days and hours. Palliative care services do indeed benefit people nearing the end of their journey, but the field has become much broader over time. Many patients with a life-threatening disease now start receiving palliative care early—sometimes soon after diagnosis..."
How to Tell Someone You’re #Terminally #Ill. #hpm
"Though everyone eventually dies, few know how to talk about the end of life. ‘‘People don’t know what to say,’’ Wanda says. ‘‘They’re afraid.’’ Be prepared for strange and stilted reactions. Some want to believe in a fix and will give you unsolicited health tips. (‘‘Don’t eat sugar.’’ ‘‘Avoid gluten.’’) You can ignore their suggestions but acknowledge the heart underlying them. People may offer to pray for you. ‘‘Prayers are good, but maybe what I need is someone to listen,’’ Wanda says. For that type of engaged listening, you may need to seek out a professional, like a trained social worker or a psychiatrist. Sometimes people who know about your condition — those you tell will tell others — will pretend your situation does not exist. Or weirder still, they will temporarily forget".
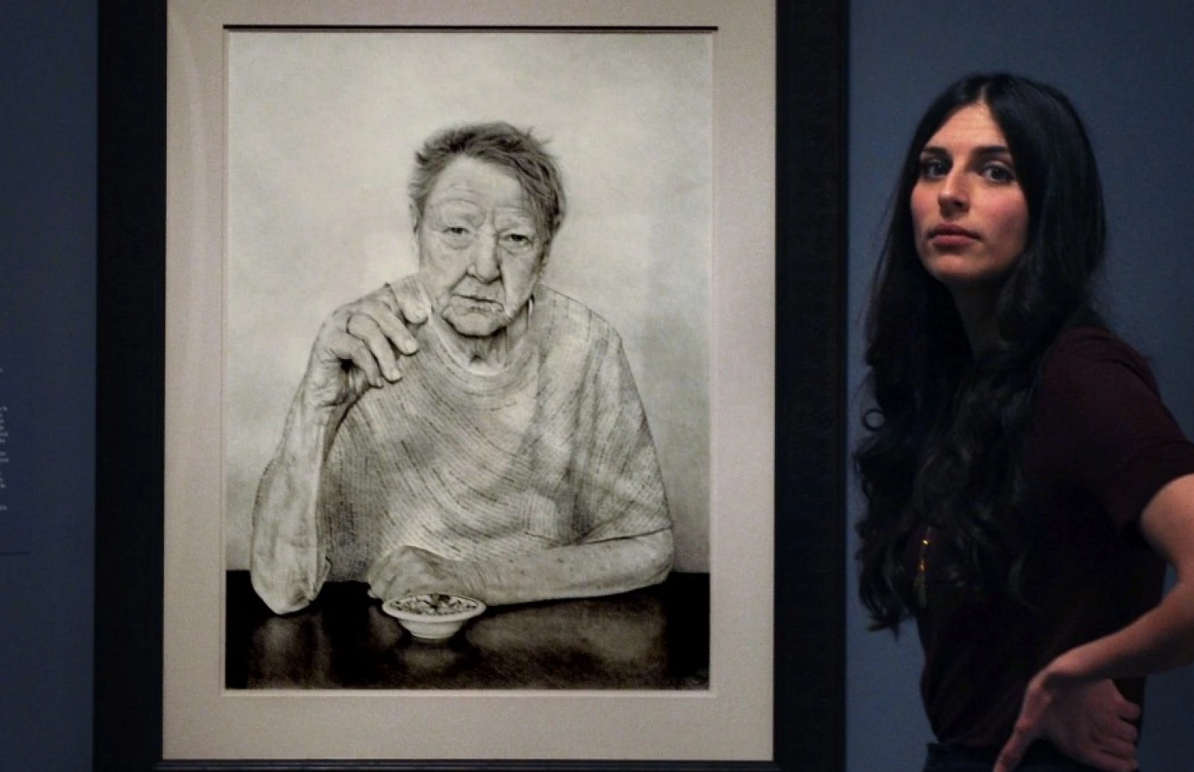
Drawing portraits of #dying people in #hospice taught this artist about #living. #hpm @claudiabicen
"Sitting in the museum’s atrium the day before the show opened, Biçen, 29, said she embarked on the project believing the dying might have lessons to teach her.
'Birth and death – these two moments of life are really sacred, and everything in between is kind of the madness of life,' she said. 'I thought that lying there on your deathbed you’re going to be confronting your life. What did it feel like to be dying? I think most people haven’t had a conversation with someone who is dying. It’s just pushed out of social consciousness and I think that’s problematic'."
How ‘Before I #Die’ Walls Boost #Palliative #Care. #hpm @candychang
" 'In order to die well, we need to learn how to talk about it,' Chang said, speaking to members of AAHPMN and HPNA.
Palliative care offers those with serious illnesses—both short and long term—more options with a focus on improving the quality of life. Public support for palliative care and end-of-life planning with medical professionals has swelled in recent years, but talking about death and care for those with serious illness is still complicated and difficult.
What Chang accomplished in her project was open up the conversations that are difficult to have—both with doctors and family members—whether under the circumstances of a serious illness or not. The chalkboards provided an anonymous outlet to share ideas, memories, anxieties and aspirations that are emotional and complicated."
‘Everything We Say and Do’: Soliciting #Goals from Our #Patients and Their #Families
“Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the 'key communication' tactics in practice to maintain provider accountability for “Everything we say and do that affects our patients’ thoughts, feelings and well-being.”
#Dying Better, Even If It Means Sooner. Delaying #death with excessive, expensive end-of-life care often does more harm than good.
"Looking back, many sons and daughters I have worked with regret having encouraged a parent to undergo a hip surgery. Spouses regret pushing for their loved ones to be intubated, and many patients struggle to balance the suffering with the life-prolonging effects of their treatments. Such regrets are the outgrowth of an approach to death that is focused on delaying death rather than being present and accompanying loved ones as they are dying. Accessing death-delaying treatments often comes at the expense of easing discomfort and being intentional about the nonmedical ways we can help our dying loved ones".
Why #Death Is Good Dinner #Conversation. #ACP @deathoverdinner @convoproject
"As I write this, I’m five years post-diagnosis and officially in “survivorship” care – I now go in for follow-up only once a year. And I have to admit, with cancer further and further in the rearview mirror, it’s easy to get back into denial mode when it comes to death – “I’m going to live forever!”
But we need to acknowledge death, talk about it, whether we’re a terminal patient, a just-diagnosed Stage I patient, or someone entering “survivorship.”
Recently, there have been the beginnings of a movement to help us all get real and have “the talk” about death.
So let’s get talking. Even if it’s scary and awkward, having this talk will greatly increase the chances that your end-of-life wishes are honored.
Death Over Dinner and The Conversation Project are organizing a week-long National Dinner Party to Dine and Discuss Death April 16 through 22".
7 Fun Ways To Teach Your #Kids #Mindfulness
"If you ever want to be inspired and also have a giggle, ask a group of kids what they think “mindfulness” is. “Relaxing out of our daily troubles and stress,” “A way to stay yourself when you’re going through something troubling” and “It’s like getting off of one railroad track and getting onto another one” were some of my favorite answers from the recent class meeting. Kids can really be fountains of spiritual wisdom!
When I told them the dictionary’s definition (“a mental state achieved by focusing one's awareness on the present moment, while calmly acknowledging and accepting one's feelings, thoughts, and bodily sensations, used as a therapeutic technique"), the kids weren’t entirely sure what I was talking about. And so we did some exercises to test it out. Feel free to try these at home!"
#Childhood #Bereavement #Care Pyramid
"In the absence of a national approach to childhood bereavement care in Ireland, the pyramid is a guide for professionals and concerned adults in identifying and responding to the needs of children and young people who have experienced a loss.
An expert group working in the area of childhood bereavement was convened to review the adult and child bereavement literature and pertinent policies (international and local), in order to establish existing models of bereavement care and core dimensions of best practice. From this review and building on practice experience, a framework was created and piloted with medical, social work and educational professionals and parents".
National #Family #Caregiver Day.
"On the first Tuesday of April, Canadians come together to recognize family members, friends, neighbours and other significant people who take on a caring role to support someone with a diminishing physical ability, a debilitating cognitive condition or a chronic life-limiting illness. Known as National Family Caregiver Day or National Carer Day, this special day encourages all Canadians to pay tribute and recognize the valuable contribution of family caregivers to our lives and our society as a whole."#Family
#Health Sentinel: Lack of #knowledge about #palliative care limiting its benefits to #patients, #hospitals. #hpm
"When Gerald’s physicians discussed options and next steps, palliative care was among them. Rozanne, a retired teacher, was familiar with hospice but unaware of palliative care as a specialized service.
'I didn’t have a clue,' she said, but added that through those services, 'our every need was met.'
Multiple studies show that, compared to awareness of hospice, “There’s significantly less familiarity with palliative care,” said Dr. Lyle Fettig, director of Indiana University School of Medicine’s Hospice and Palliative Medicine Fellowship program centered in Indianapolis…
Palliative care, according to the New York-based Center to Advance Palliative Care, is appropriate for any age individual and at any stage of a serious illness, whether that illness is cancer or a chronic condition, such as heart or lung disease. The goal is to improve quality of life for both patient and family through a holistic, interdisciplinary team approach”.
#Death and the #Workplace. @GroundSwellAus
"We know that most of us don’t grieve in stages. In fact, we experience resilience. To use George Bonnano’s research, for most of us grief is an up and down experience with capacity for both intense positive and negative emotion. This is normal and expected. And perhaps most importantly, we know that being part of a network of colleagues (as well as friends and family) who take part in the caring process, has a transformative effect. Not just for those of us who are experiencing great loss, but also for the people who work with and care for us."
The importance of #honest #communication: Talking with #children about #death. #hpm
"Drawing from over 30 years of stories and wisdom from grieving children, teens, and adults, the Dear Dougy Podcast is opening up the conversation about dying, death, and bereavement. As humans, we all experience loss during our lives, but often find ourselves lost and unsure when it comes to navigating the grief that follows. Whether you’re grieving a death, or wanting to support someone who is, the Dear Dougy Podcast can help explore your questions about grief".
Repeat After Me: 'Hospice Means More Care, Not Less.'
"If you or anyone you know has advanced illness that isn't meaningfully getting better (or keeps getting worse) in spite of many treatments and hospital stays and doctors' visits then you owe it to yourself to learn more about hospice sooner rather than later. This is especially true for more frail elders with serious illness because the hazards of additional hospitalizations and certain treatment side effects are more serious and more common. Ideally, hospice care is set up on a better day, in advance of a true crisis so that the hospice team and person receiving services can get to know one another and set up truly personalized care. Too many people elect hospice so late in their course of illness that they miss out on many of the benefits".
How to Talk About Dying.
“Too many people we love had not died in the way they would choose. Too many survivors were left feeling depressed, guilty, uncertain whether they’d done the right thing.
The difference between a good death and a hard death often seemed to hinge essentially on whether someone’s wishes were expressed and respected. Whether they’d had a conversation about how they wanted to live toward the end…
We still need to transform the cultural norm from not talking about how we want to live at the end of life to talking about it. The real work to close the gap is not just for doctors and patients. It’s for mothers and daughters, husbands and wives, families and friends. We have to bring people to the kitchen table to talk with those they love to have the conversation. And to do this before there is a crisis. Not in the I.C.U.”
In #Palliative #Care, #Comfort is the Top Priority. #HPM
"Although 40 percent of their palliative care patients can expect to be cured, 'there clearly still are both patients and oncologists who have an inappropriate association in their minds,' he said. 'They still associate palliative care with giving up.'
To the contrary, palliative care can help patients live fully, regardless of their prognoses."
This is not Casualty – in real life #CPR is brutal and usually fails. #ACP #Awareness
"Modern medicine, however, still shies away from discussions about natural death and dying, and is more comfortable in the realms of what can be done. Doing something always trumps doing nothing. Healthcare professionals have become willing interventionists, and we cannot stop meddling, interfering and attempting to fix.
Many people I speak to presume that if the label “Not for CPR” or “DNACPR” (Do Not Attempt CPR) is added to their notes, this might preclude them from other resuscitative treatments such as antibiotics, fluids and blood transfusions. Dispelling this myth takes time and reassurance. Patients can still have active, resuscitative measures if they become increasingly unwell, but remain not for CPR for when their heart stops".
A Loud Voice: Dear Dead Mother. Conversations about #life, #love, and #loss with the mother I've never known. #Grief #Bereavement
"Silence is not always self-imposed. Sometimes those of us who want to grieve out loud feel immense pressure to stay quiet and move on. This pressure can be communicated to us in so many ways – when people look away, when words are whispered across quiet rooms, when we are explicitly told not to dwell on negative things. When the people we love most and want to protect seem to fall apart when we talk about the dead".