About Childhood Grief
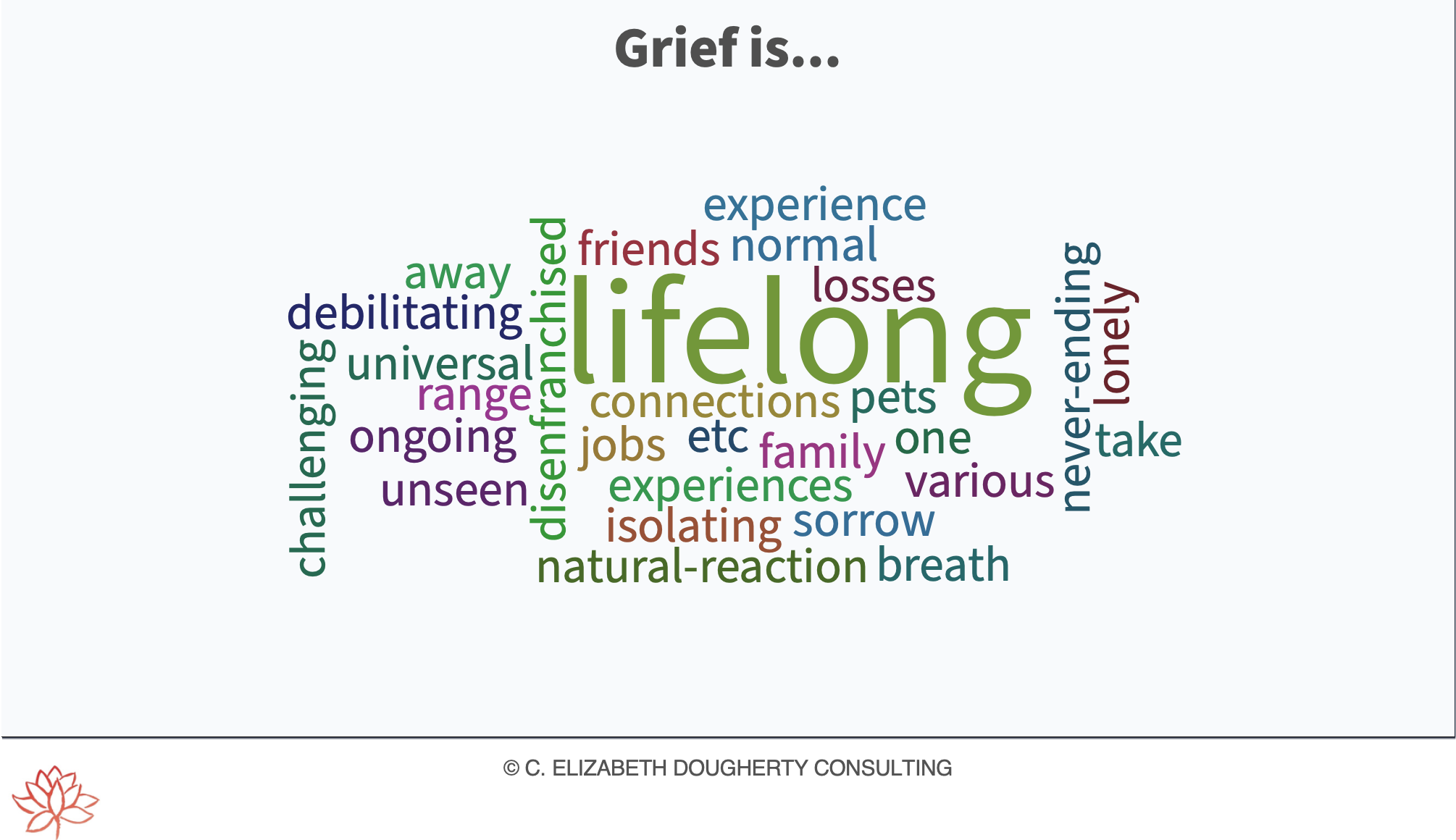
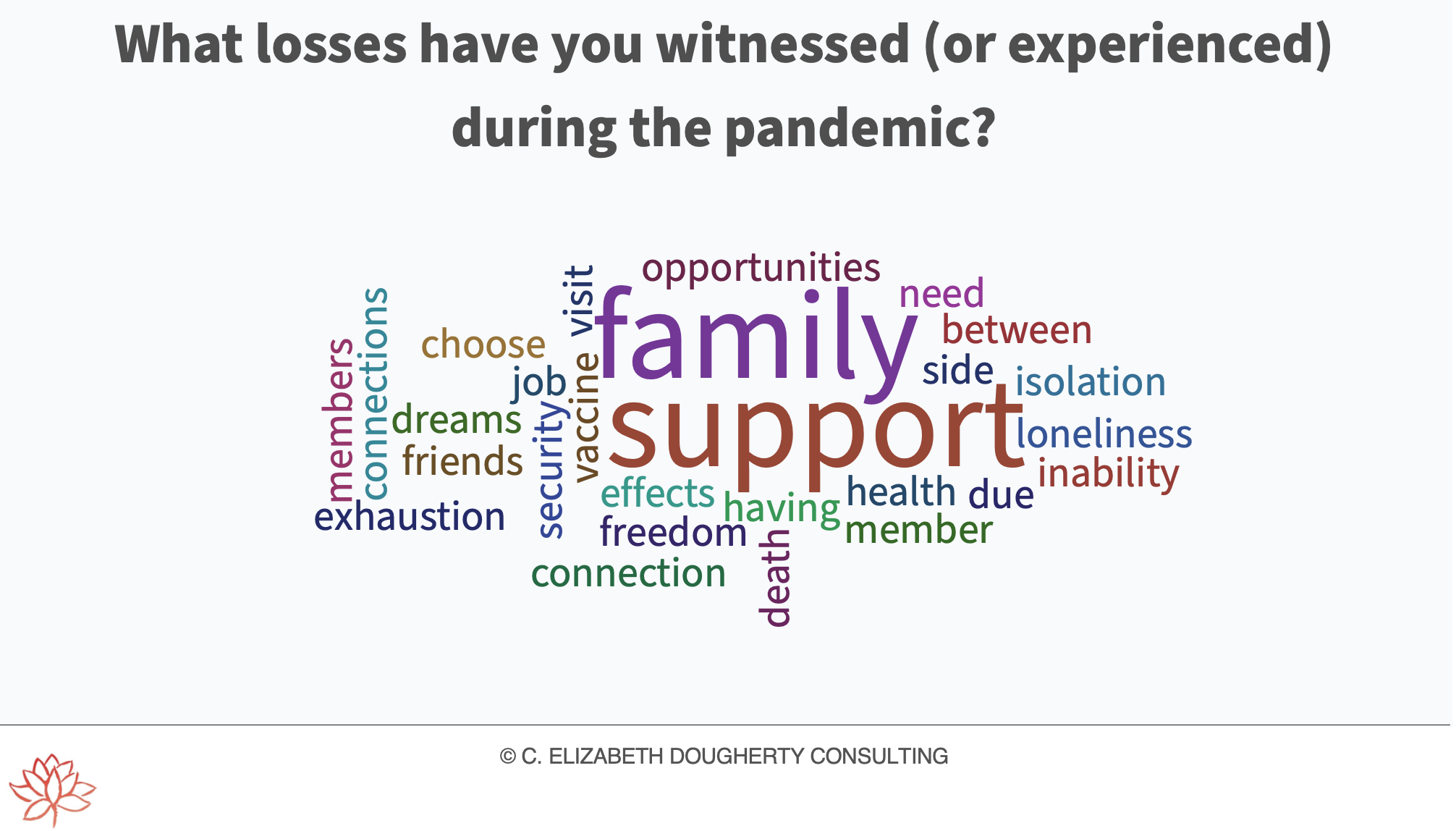
“The death of a family member, friend or other significant person is a lifelong loss for children. It is normal for children to miss the person who died and to experience grief that might come and go with different levels of intensity for some time after the death. It can be challenging to parents and caregivers to know what to do for, what to say to and how to help children who are obviously hurting. Here are a few suggestions about how to be helpful to a grieving child based on research and practice among children’s grief support professionals and volunteers. It is important to note that grief reactions in children are varied, wide ranging and unique to each individual.”
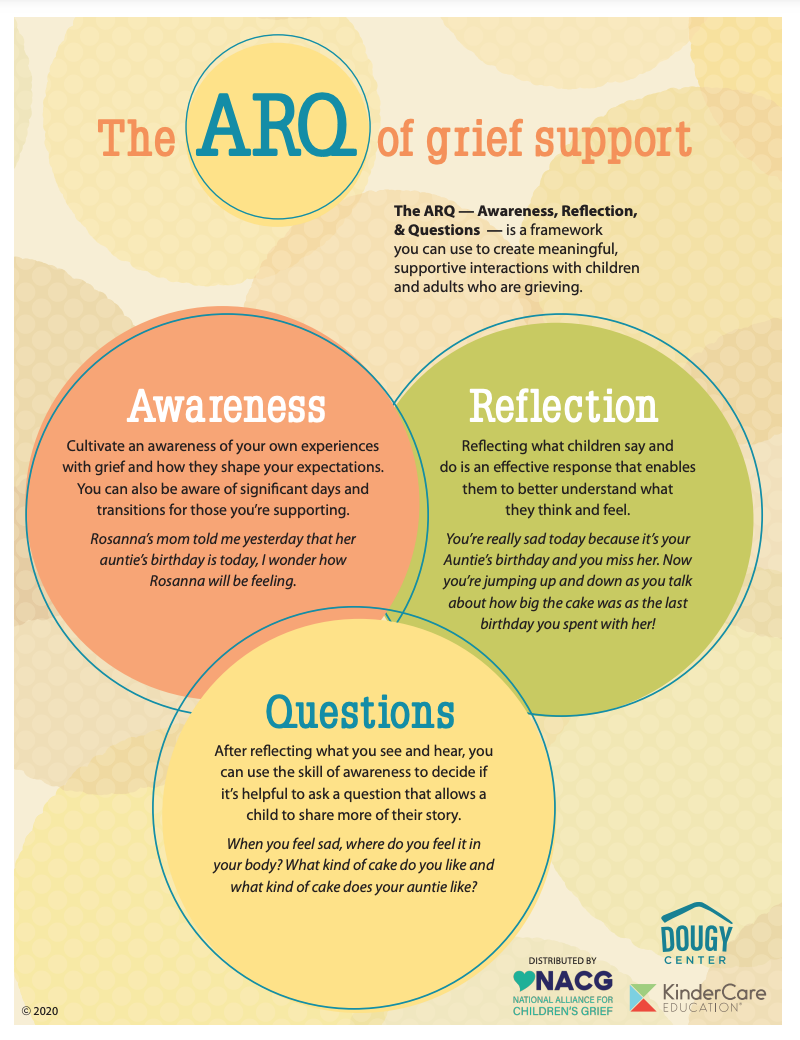
The following suggestions will help guide you as you seek to be provide understanding and compassion to children living with grief:
Grief is a normal reaction for children to the death of someone significant
Children need to know the truth. Most parents and caregivers would agree that they would prefer that their children not have to deal with the difficult truths that might accompany a death
Each child’s grief is as unique to him or her as was their relationship with the deceased
Grieving children often feel alone and misunderstood
Children will experience grief over the death of significant people at different times throughout their lives
Grieving children often experience personal growth as a result of their loss
Grieving children feel less alone when they are with other children who have experienced the death of a significant person and when they have loving, consistent adults in their lives
Knowledge is Power
Source “About Childhood Grief” via NACG