Hospice care: 'This is what dying should look like'. #HPM
"The goal of the hospice and palliative care is to minimize the suffering of the patients and their families and to make the best of their last days".
"Before I go". ~ Dr. Paul Kalanithi
"Time for me is double-edged: Every day brings me further from the low of my last cancer relapse, but every day also brings me closer to the next cancer recurrence — and eventually, death. Perhaps later than I think, but certainly sooner than I desire. There are, I imagine, two responses to that realization. The most obvious might be an impulse to frantic activity: to “live life to its fullest,” to travel, to dine, to achieve a host of neglected ambitions. Part of the cruelty of cancer, though, is not only that it limits your time, it also limits your energy, vastly reducing the amount you can squeeze into a day. It is a tired hare who now races. But even if I had the energy, I prefer a more tortoiselike approach. I plod, I ponder, some days I simply persist".
How one couple’s loss led to a push for psychological care for kids with cancer.
"The standards say families should be educated early on about palliative care and its role in helping to “reduce suffering throughout the disease process.” And they say children with cancer should receive “developmentally appropriate” information to prepare them for the treatments and procedures they will undergo".
Patients aren’t told that death is near until too late. We can do better.
"Oncologists, cardiologists, and other specialists can often predict a patient’s rate of decline based on a specific disease, Obermeyer said. But patients, particularly those who are elderly, often suffer from more than one serious illness that make it more difficult to predict when they’re near death. So a pulmonologist might treat someone’s pneumonia, for instance, without recognizing it signals a broader decline".
"A parting lesson from my parents". ~Andrew Dreyfus
"As I have become more involved with this work, I have wondered whether the CEO of a large health plan is the right person to talk about end-of-life care. But I only have to remember how important this issue was to my brother and my parents to realize that — in this case at least — my personal experience should inform my professional actions. Everyone, regardless of economic, cultural, racial, or geographic differences, must have their choices and values heard and respected. Everyone deserves the chance to live the best life possible, to the very end".
Dignity, Respect and Choice: Advance Care Planning for End of Life for People with Mental Illness.
"Dignity, Respect and Choice: Advance Care Planning for End of Life for People with Mental Illness is a two part resource that will help support people with mental illness, their families and carers, and health professionals with the complex issues which might arise around Advance Care Planning for End of Life".
What Would You Write If You Knew You Were Dying?
This talk was given at a local TEDx event, produced independently of the TED Conferences. Writing for the future. Recording conversations Rachel has a passion for honest conversations, and recognises the precious and precarious nature of life. She supports families when an adult develops cancer and helps those at the end of life to tell their story.
"When life runs out of tomorrow's, what you realize you've got is today" ~ Rachel L. Smith
Before the tomorrow's run out, use this opportunity today to think about what you will you say to your loved ones... And then say it...
Toward Evidence-Based End of Life Care. ~NEJM
"The disquieting patterns of end-of-life care in the United States have been well documented. In the last month of life, one in two Medicare beneficiaries visits an emergency department, one in three is admitted to an intensive care unit, and one in five has inpatient surgery. But one of the most sobering facts is that no current policy or practice designed to improve care for millions of dying Americans is backed by a fraction of the evidence that the Food and Drug Administration would require to approve even a relatively innocuous drug".
Child and Youth Grief Awareness: Resources.
Children's Grief Awareness Day.
"Children's Grief Awareness Day seeks to bring attention to the fact that often support can make all the difference in the life of a grieving child. It provides an opportunity for all of us to raise awareness of the painful impact that the death of a loved one has in the life of a child, an opportunity to make sure that these children receive the support they need".
Finding the Words: How to talk with children and teens about death.
"It's hard to talk to children and teens about death and dying, particularly when someone they love has died or might die soon. Our instinct as caring adults may be to shelter them from painful truths. Yet as Dr. Wolfelt emphasizes, what kids need most is our honesty and our loving presence.
This practical and compassionate handbook includes dozens of suggested phrases to use with preschoolers, school-agers, and teenagers as you explain death in general or the death of a parent, a sibling, a grandparent, or a pet. Other chapters include possible words and ideas to draw on when you are talking to kids about a death by suicide, homicide, or terminal illness. At times grown-ups must also have very difficult conversations with dying children; this book offers guidance. A final chapter discusses how to talk with kids about funerals, burial, and cremation".
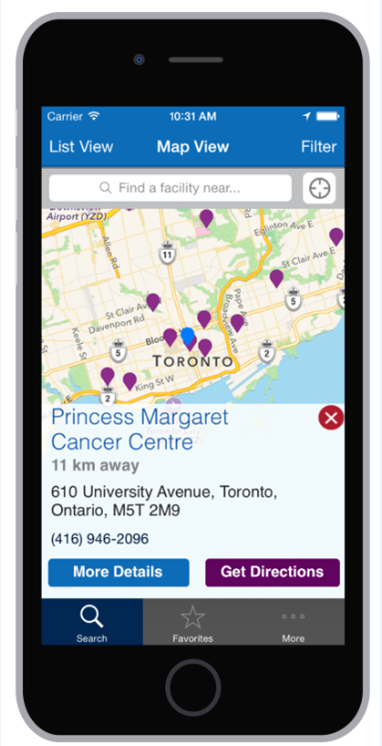
Inpatient Hospice Palliative Care Directory free via iOS and Android.
"Although some people hope to remain at home for the duration of their illness, many people find that admission to an inpatient setting can also be helpful. The inpatient care settings in the directory include palliative care units, residential hospices and dedicated palliative care beds within local hospitals. Inpatient hospice palliative care support includes 24 hour care, specialist pain and symptom management and psychosocial support for patients and families.
The map provides access to a directory which includes more information about inpatient hospice palliative care settings across Ontario. The list of facilities below may not be complete - there may be hospice palliative care settings which are not in the directory.
For contact information and details about the facility, click on a specific location. If you want more information, contact the hospice or palliative care program directly".
Bearing Witness to Suffering. ~ Laura van Dernoot Lipsky
In this talk, Laura offers us a window into the cumulative toll that can occur when we are exposed to the suffering, hardship, crisis or trauma of humans, other living beings, or the planet itself. Held within a larger context of systematic oppression and liberation theory, we'll dive into what gets hard and how to work toward reconciling it both individually and collectively.
Advance Care Planning. Speak Up!
"Advance Care Planning is a process of reflection and communication. It is a time for you to reflect on your values and wishes, and to let people know what kind of health and personal care you would want in the future if you were unable to speak for yourself.
It means having discussions with family and friends, especially your Substitute Decision Maker – the person who will speak for you if you cannot speak for yourself. It may also include writing down your wishes, and talking with healthcare providers and financial or legal professionals"
Click on the above image to learn more.
The Way Forward: An Integrated Palliative Approach to Care.
Palliative Care Sooner for Patients But Also for Medical Professionals.
"Changing culture is a process. Awareness and understanding of palliative care is often limited, yet the benefits are discernible from better quality of life to care more consistent with patient preferences, to more recent data indicating improved survival. My experience with palliative medicine as a first-year medical student has made me realize how vital palliative care education could be for all medical students".
Complicated Grief: A Grief So Deep It Won’t Die.
" 'Adapting to loss is as much a part of us as grief itself,' said Dr. Shear, who directs the Center for Complicated Grief at the Columbia University School of Social Work. With complicated grief, 'something gets in the way of that adaptation, Something impedes the course of healing.’
By diagnosing complicated grief just six months after a death, he said, 'you’ll get a lot of normal people receiving treatment they don’t need,' including drugs. Dr. Shear also worries about “pathologizing” normal emotions. But when a woman remains unable to leave her home or answer the phone four years after the death of her adult son, as was true of one patient, something has clearly gone wrong.
‘If you’re worried about what you’re experiencing, if you’re not getting more engaged in life and people around you are saying, ‘Honey, stop wallowing in it,’ why not get some help?' Dr. Shear said. Complicated grief therapy, developed by her center, showed greater effectiveness among older adults than interpersonal psychotherapy in a clinical trial".
The Paternalism Preference — Choosing Unshared Decision Making.
"Consent is not merely the granting of permission but an exercise in choosing, and choice requires disclosure of a certain amount of information. How much information is adequate? Rather tautologically, as much as necessary to decide: 'The scope of the physician's communications to the patient must be measured by the patient's need, and that need is whatever information is material to the decision'.”
Grief Through a Child's Eyes.
Click on the above image to watch "Grief through a Child's Eyes" an original video that takes you inside a children's bereavement camp.